- About MOPH
- Laws and Regulations
- Administrative Services
- E-Services
- Publications
-
Media Center
links

- Beirut Summit 2019
- National Organization for Organ and Tissues Donation and Transplantation
- Ministry of Agriculture
- Ministry of Culture
- Ministry of Displaced
- Ministry of Economy and Trade
- Ministry of Education and Higher Education
- Ministry of Energy and Water
- Ministry of Environment
- Ministry of Finance
- Ministry of Foreign Affairs and Emigrants
- Ministry of Justice
- Ministry of Industry
- Ministry of Interior and Municipalities
- Ministry of Labor
- Ministry of National Defense
- Ministry of Public Works and Transport
- Ministry of Social Affairs
- Ministry of Telecommunications
- Ministry of Tourism
- Ministry of Youth and Sports
- Office of the Minister of State for Administrative Reform (OMSAR)
- Rafic Hariri University Hospital (RHUH)
- Central Administration of Statistics (CAS)
- Civil Service Board
- Cooperative of Government Employees
- Council for Development and Reconstruction
- National Council for Scientific Research
- National News Agency
- National Social Security Fund
- Lebanese Order of Physicians
- Order of Pharmacist
- Order of Nurses in Lebanon
- Syndicate of Hospital in Lebanon
- Europian Union
- International Medical Statistics (IMS)
- United Nations
- The World Bank
- World Health Organization (WHO) office in Lebanon
- World Health Organization (WHO)
- Track Your Document
- Drugs Public Price List
- Health Facility Locator
Related sites
- Beirut Summit 2019
- National Organization for Organ and Tissues Donation and Transplantation
- Ministry of Agriculture
- Ministry of Culture
- Ministry of Displaced
- Ministry of Economy and Trade
- Ministry of Education and Higher Education
- Ministry of Energy and Water
- Ministry of Environment
- Ministry of Finance
- Ministry of Foreign Affairs and Emigrants
- Ministry of Justice
- Ministry of Industry
- Ministry of Interior and Municipalities
- Ministry of Labor
- Ministry of National Defense
- Ministry of Public Works and Transport
- Ministry of Social Affairs
- Ministry of Telecommunications
- Ministry of Tourism
- Ministry of Youth and Sports
- Office of the Minister of State for Administrative Reform (OMSAR)
- Rafic Hariri University Hospital (RHUH)
- Central Administration of Statistics (CAS)
- Civil Service Board
- Cooperative of Government Employees
- Council for Development and Reconstruction
- National Council for Scientific Research
- National News Agency
- National Social Security Fund
- Lebanese Order of Physicians
- Order of Pharmacist
- Order of Nurses in Lebanon
- Syndicate of Hospital in Lebanon
- Europian Union
- International Medical Statistics (IMS)
- United Nations
- The World Bank
- World Health Organization (WHO) office in Lebanon
- World Health Organization (WHO)
Hotline for Health Services for Displaced Lebanese 1787Hotline for the Patient Admission to Hospitals 01/832700COVID-19 Vaccine Registration Form covax.moph.gov.lbMoPH Hotline 1214
Are you a new member? Sign up now
- CHANCE Association Concludes Its Project on Innovation in Pediatric Tumors
- Quality Assurance of Pharmaceutical Products
- Estimated Resident Population
- The Lebanese University of Arts and Sciences (USAL) Launches the Project “Leaders Against Drugs"
- Nassereldine with the Korean Ambassador and the UNICEF Representative Inspected Al-Zahraa Center
- Pandemic Fund Lebanon Project: Using the One Health Approach To Drive Resilience and Recovery
- Updated List of Pharmacies Connected to "Meditrack System"
- Updated List of Pharmacies Connected to "Meditrack System"
- Drugs & Pharmaceutical like Registration
- MediTrack Project - Track & Trace System for Pharmaceuticals
- Latest News
- Nassereldine Signs a Memorandum of Understanding with the Modern University for Business and Science (MUBS)
- The American University of Cyprus Graduates the First Cohort of the Public Health Pioneer Program
- Nassereldine Launches Lebanon’s Sustainable Food-Based Dietary Guidelines
- Nassereldine at the Opening of the "Beirut International Breast Cancer Conference"
- Nassereldine Launches the “Kareem” Initiative to Give Full Health Coverage to Displaced Residents in Tripoli
- Nassereldine Launches Hospital Coverage for Stroke
- Thirteen Dead and Eight Injured in Building Collapse in Tripoli
- Nassereldine Put the Foundation Stone for the Rehabilitation Works of the National Central Laboratory
- National Cancer Prevention Awareness Campaign 2026
- Nassereldine from Shheem: The Number of Cancer Cases in Lebanon are Alarming and Early Diagnosis is Key
- Request for Pharmacist for the National E‑Health Program
- World Cancer Day at MoPH: Testimonials of Life and Presentation of Future Plans
- Drugs Technical Committee
- Medical Devices Recalls
- Minister of Health Inaugurates "Lebanon Medical Center" in Hadath
- MoPH Coverage for Medical Expenses of the Injured of the Building Collapse in the Tabbaneh Area
- The Ministry of Public Health is Surprised by the Kuwaiti Statement
- Nassereldine from Dar El-Hikma Hospital - Baalbek:We Deal with our Ministries with Patriotism
- Nassereldine Tours the "Lebanon Medical Center"
- Nassereldine Inaugurates the "Barja Ambulance Center": Regulating the Sector is a Priority
- National Conference at USEK to Develop an Integrated Strategy for Medical Tourism in Lebanon
- Nassereldine Visits the Children's Cancer Center
- Drugs Public Price List 2026
- Infant Formulas (from 0 to 1 year)
- Nassereldine Visits Barbara Nassar Cancer Center, Endorsing its Slogan "No Begging, No Pleading"
- Lebanese Guideline on Good Pharmacovigilance Practices (LGVP)
- MoPH and UNICEF Accredited Three Baby-Friendly Hospitals in Lebanon
- NCR graphs - Incidence rates by year
- NCR Graphs 2005-2024
- NCR graphs - Age specific incidence rates
- NCR graphs - Incidence rates by site
- National Pharmacovigilance Program Newsletter - Issue 17 -January 2026
- Statement Issued by the Ministry of Public Health
- Pharmacovigilance System in Lebanon
- Updated List of Pharmacies Connected to "Meditrack System"
- Nassereldine Inaugurates the "Empowering Hospital Pharmacists" Program
- Request From Nassereldine: 100% Health Coverage for Displaced People from the Southern Border Villages
- Nassereldine Open The 2nd Middle East Genitourinary Oncology Conference at AUBMC
- Ministers of Public Health and Social Affairs Announce the Health Coverage Mechanism for Displaced People
- Junior Public Health Officer
- NCR Tables 2005-2024
- NCR tables - Incidence
- NCR tables - Distribution of cases by age and site
- NCR tables - Counts of cases
- Nassereldine Follows up with the World Bank on Current Health Projects
- General surveillance data: past years
- Nassereldine Inaugurates the Imam Hussein Center in Burj al-Barajneh
- Nassereldine Inaugurates the Fasting and Health Conference
- Nassereldine Gives Instructions to Treat the Injured of the Collapsed Building in Qoubbeh Tripoli
- Nassereldine Representing H.E.Berri Inaugurates the Endoscopy & Oncology Departments at Al-Zahraa
- Closure of Two Chicken Warehouses in Saadnayel for Violating Food Safety Regulations
- Nassereldine Represents the PM at the Conference on Innovative Breakthroughs in Dermatology and Oncology
- Nassereldine Congratulates Dr. Maha Hoteit on Her Selection as One of the WHO's Elite Experts
- National Cancer Registry (NCR)
- Nassereldine Sponsors the Launch of "Banin" Association's "10452 Initiative"
- The Ministers of Public Health and Environment Inaugurate the Infectious Medical Waste Treatment Center in Karantina
- National Digital Health Transformation Strategy 2025-2030
- Nassereddine Met a Delegation from the European Union Mission, the Colombian, and Korean Ambassadors
- Issuance of a Report on the Adverse Events Following Medications and Vaccines Use in Lebanon
- Nassereddine Launches the Updated Version of the MOPH Mobile APP
- Issuance of a New Drugs Public Price List
- Drugs Public Price List 2025
- Drugs Public Price List 2024
- New Hospitals Join the MediTrack System
- Updated List of Pharmacies Connected to "Meditrack System"
- List of PHCCS Within the MoPH Network that Have an Operating Psychiatrist
- Drugs Recalls
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.2/1 & 4/1 & 5/1 Date 5/1/2026
- Annual Newsletters
- Reports and Publications
- National PHC Network
- Narcotics
- List of Contact Lenses and Solutions for Contact Lenses Approved from MoPH
- Press Release about Seasonal Influenza
- Nassereddine and the Chinese Ambassador Discuss Strengthening Cooperation in Health and Hospital Projects
- Nassereddine Was Honored at Hôtel-Dieu in Recognition of his Continued Support for Health Institutions
- Sustainable Development Goals (SDG)
- Vital Data Observatory Statistics
- Nassereddine Inaugurates "St.Veronica Medical Center" at the Monastery of Our Lady of the Annunciation - Zouk Mikael
- Nassereddine Inaugurates the Renovated Floor at Dr. Emile Bitar Hospital in Batroun
- Nassereddine at the Annual Meeting of PHC Centers: We are Moving Forward to Support the PHCs Financially
- The Ministry of Public Health Launches the Updated Version of Its Mobile APP
- Nassereddine at a Seminar on "The Impact of Technology on Clinical Research"
- The National Campaign on Adolescent Health- 2025
- Launching of the First National Campaign on Adolescent Health in Grand Serail
- Nassereddine Inaugurates the CT Scan Machine at Hariri Hospital and Honors its Employees
- Memorandum of Understanding between MoPH and AstraZeneca for the Early Diagnosis of Lung Cancer
- Salam Launches a Plan from the Grand Serail to Equip Governmental Hospitals
- Nassereddine during a Meeting with Hospital Directors in Baalbek
- Download the Official MOPH Mobile App: (New version)
- Nassereddine Inaugurats the Scientific Conference at Sagesse University on the Future Medical Imaging
- Nassereddine Accompanies President General Joseph Aoun on a Visit to the Sultanate of Oman
- MoPH will Announce its Comprehensive Plan for Equipping Governmental Hospitals
- Nassereddine Visits Governmental Hospitals and PHC Centers in West Bekaa and Rashaya
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2285/1 Date 26/11/2025
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2196/1 Date 18/11/2025
- Nassereddine and the Japanese Ambassador Sign a Japanese Grant to Strengthen the Public Health Sector
- Workshop on "Health Facilities in Akkar in Relation to Climate Change"
- A Workshop on "Health Facilities in Akkar in Relation to Climate Change" Was Held
- Laboratory Technician Competence Exams Scheduled for Students Applying for Professional Practice License
- Issuance of the Results for the Laboratory Technician Exams for Professional Practice License
- Nassereddine Opens the Prostate Cancer Control Conference
- Nassereddine Opens the Cellular and Immunotherapy Conference: We are Entering a New Era in Oncology
- Nassereddine on the Occasion of World AIDS Day: The Drug is Available with the Support of Partners
- Nassereddine Inaugurates The Humanization of Innovation in Artificial Intelligence Center at the Islamic University
- Nassereddine Inaugurates the Service Improvement Project in the Karagheuzian PHC Center with Support from Japan
- Public Health Emergency : 335 Martyrs and 973 Wounded since the Signing of the Ceasefire Agreement
- Nassereddine and the Indian Ambassador Sign an Agreement to Rehabilitate the PHC Center at Qana Gov. Hospital
- Nassereddine Places a Rose Wreath at the Tomb of Sabri Hamadeh in Hermel
- Nassereddine Inaugurates the Martyr Ali Allam Medical Center in Baalbek
- Nassereddine Launches the Lung Cancer National Awareness Campaign
- Nassereddine Launches the Lung Cancer National Awareness Campaign
- Lung Cancer Awareness Campaign 2025
- Public Health Emergency Operation Center: 331 Martyrs and 945 Wounded since November 28th
- National Campaign to Awareness-Raising Drowning Prevention"- 2025
- MoPH Condemns the Attack on a Nurse at Tripoli Governmental Hospital
- Nassereddine Sponsors the Launch of the Social Child Clinic, the First Program for Early Detection of Scoliosis
- Nassereddine Visits the Sir Denniye Governmental Hospital and Primary Healthcare Centers
- Hospital-based Cause Of Death Notification System
- Standards for Daycares
- Updated List of Pharmacies Connected to "Meditrack System"
- National Pharmacovigilance Program Newsletter - Issue 16 -October 2025
- National Pharmacovigilance Program Newsletter - Issue 16 -October 2025
- Nassereddine and Haidar Inaugurate the "Chronic Care Center" Conference in Baabda
- Nassereddine Sponsors the Opening Ceremony of the Chemotherapy Center at Hiram Hospital in Tyre
- Nassereddine Receives a Lebanese Medical Team from Detroit to Perform Free Surgeries in Lebanon
- List of Certified Warehouses in Compliance to GSDP Guidelines
- Educational Workshop for Media Professionals at MoPH on Cervical Cancer Prevention
- Workshop on "Strengthening Ministerial Cooperation in the Fields of Health and Social Services"
- Nassereddine:By Combining our Efforts and Cooperating with our Expatriate Communities, We Will Build our Lebanon
- Nassereddine Sponsors a Health Day in Hermel
- List of Registered Implantable Medical Devices at MOPH
- Nassereddine from Zahle: Covering the Costs of Prosthetics for Pelvic and Hip Fractures for Elderly
- Nassereddine Opens the MUBS Regional Conference on "Accreditation and Infection Control"
- The Ministers of Health and Information Launch the Free Guide "Know Your Health Rights"
- President Aoun Discusses with Nassereddine the Health Situation in Lebanon
- Nassereddine Signs an Agreement with the French Development Agency
- Updated List of Pharmacies Connected to "Meditrack System"
- Request for Procurement and Installation of Medical Furniture
- Organizing a Competition to Contract with Controlling Doctors for the Ministry of Public Health
- Nassereddine Sponsors the Opening of a Medical Conference at Al-Batoul Hospital
- Nassereddine at the Opening of a PHC Center in Ghaziyeh
- Nassereddine Meets with Poland Ambassador
- Nassereddine Discusses the Strategic Partnership with a Delegation from the Qatar Fund for Development
- Nassereddine Opens a Scientific Conference on Palliative Care
- Nassereddine Relaunches the National Campaign for Awareness and Early Detection of Breast Cancer
- National Breast Cancer Awareness Campaign 2025
- Mikati at the Opening of the Dialysis Center at Minia Governmental Hospital
- National Breast Cancer Awareness Campaign 2018
- Nassereddine Reopens the Mental Health Unit at Rafik Hariri University Hospital
- Nassereddine Announces that October 20th Will Be the National Osteoporosis Day in Lebanon
- Updated List of Pharmacies Connected to "Meditrack System"
- Nassereddine Announces the Launch of Health Projects and a 20% Increase in Hospital Coverage in Hermel
- Nassereddine Speaks at the First Medical Conference of Saint George Hospital about Endocrinology
- Nassereddine Announces that Tannourine Company Has Been Allowed to Resume Production of Water
- Workshop on Reforms in the Pharmaceutical Sector
- MoPH Condemns the Attack on the Medical Staff at Sir Denniye Governmental Hospital
- MoPH Clarifies the Investigation into Tannourine Water Company Products
- Nassereddine:Tannourine Water Issue is a Technical Health Issue
- Nassereddine Appeals from Cairo the International Community to Renew the Support for the Health System
- MoPH-ALMA-IOM Newsletter V.1-Iss.1 2025-2026
- MoPH-ALMA-IOM Newsletter V.1-Iss.1 2025-2026
- Updated List of Pharmacies Connected to "Meditrack System"
- Statement Issued by the Minister of Public Health
- Nassereddine in Germany to Represent Lebanon at the World Health Summit
- MoPH Issues a Decision to Suspend the Operations of Tanourine Water Company
- Updated List of Pharmacies Connected to "Meditrack System"
- Updated List of Pharmacies Connected to "Meditrack System"
- The First Lady's Meeting with Young Men and Women for Mental Health Month
- Nassereddine Delivers Lebanon's Speech at the Islamic Cooperation Conference in Jordan
- Health Technology Assessment (HTA)
- Child Safeguarding Policy for Private Daycares
- Infant and Young Child Feeding
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1726/1 Date 24/9/2025
- Nursery Registration Process
- President Aoun Was Briefed by Minister Nassereddine on the Results of the Mental Health Summit in Qatar
- Nassereddine:Broad Support for Halba Governmental Hospital and a New Governmental Hospital Project in Akroum
- Nassereddine Visits Akkar
- Nassereddine Launches the Nutritional Guideline for Pregnant and Lactating Women
- Nassereddine Represents the President of the Republic at the Opening of a Medical Conference at the AUB
- Surveillance data
- Nassereddine Represents the President of the Republic at the Opening of Beirut International Dental Meeting
- Nassereddine Continues his Meetings in Qatar and Meet with his Egyptian and Bahraini Counterparts
- Nassereddine Meet the Secretary-General of the Red Crescent and Qatar Charity in Doha
- Nassereddine Visits the Qatar Cancer Society
- Nassereddine Continues his Visit in Qatar and met the Minister of Health & the Director of the Development Fund
- Nassereddine Participate in the Mental Health Summit in Qatar and met the Regional Director of the WHO
- The Lancet Journal Predicts that Lebanon will Top the Cancer Mortality Rate by 2025
- Nassereddine Inaugurates the 10th International Conference of the Syndicate of Medical Laboratory Owners
- Nassereddine Inaugurates the Psychiatric Department at Saint Charles Hospital
- List of Reference Laboratories
- Good Manufacturing Practices for Pharmaceuticals in Lebanon
- A Ceremony Was Held at the Lebanese University to Award Certificates to Graduates of the Faculty of Health
- Nassereddine Meet the Japanese Ambassador and the Group of Health Professions Syndicates
- Health Workforce
- Nassereddine Launches the Influenza Vaccination Campaign at Hariri Hospital
- Nassereddine Visits War-Wounded Children Being Treated under the "Stronger" Program
- Nassereddine Sponsors the Cooperation Agreements;Jezzine with HDF and Batroun with St George Hospital
- MoPH Honors MP Bizri "in Appreciation of his National Career in Serving Public Health"
- Nassereddine and Morcos Visit the Injured Amani Sharara at AUBMC
- School Health
- Issuance of the Lists of Public and Private Hospitals Certified For the UHID Registration updated on 22/09/2025
- Nassereddine Inspects Nazih Al-Bizri Primary Health Care Center
- Abdallah: A Successful Visit by Nassereddine to Sibline Governmental Hospital
- Nassereddine Visits the Turkish Hospital, Saida Governmental Hospital and Health Centers
- Nassereddine Inspects Sibline Governmental Hospital
- Nassereddine with Bahia Al Hariri Inspect the Hariri Foundation Social & Medical Center in Sidon
- Nassereddine Visits the Turkish Hospital, Saida Governmental Hospital and PHC Centers
- Nassereddine Visits the Hussein Medical Center in Sidon
- Cooperation Agreement Between MoPH and AUB to Enhance the Efficiency of Governmental Hospitals
- Nassereddine Inaugurates the CT Scan Machine in Dahr El Bacheck Hospital
- School Health
- The "Cedar" Award Honors the Nurses in Lebanon
- Maternal and Neonatal Health
- Protocols of the Treatment of Confirmed or Suspected Cases of Coronavirus among Pregnant Women
- The "Pager" Wounded in the Celebration of "World Patient Safety Day"
- Updated List of Pharmacies Connected to "Meditrack System"
- Request for Bids for Procurement of Laboratory Equipment for the Central Lab
- Demographic and Socioeconomic Determinants
- Nassereddine: Healthcare Centers Are the First line of Defense for the Resilience of the Lebanese
- Al-Qattan Receives Nassereddine in Bar Elias
- Nassereddine Signs a Cooperation Agreement with the Mérieux Foundation
- Nassereddine Visits Bar Elias Hospital
- The Order of Nurses in Lebanon Thanks HE Nassereddine for Approving the Two Decrees Regulating the Profession
- Be Part of Patient Safety Day 2025: Display Awareness Videos in Your Hospital
- Updated List of Pharmacies Connected to "Meditrack System"
- Updated List of Pharmacies Connected to "Meditrack System"
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1574/1 Date 3/9/2025
- Bayrakdarian and the Children's Cancer Center Launche the ByeBike Initiative from Paris to Beirut
- Nassereddine Visits the Chronic Care Center
- Nassereddine and a World Bank Delegation Visit the Al-Naqaa Primary Care Medical Center
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1598/1 & 1599/1 Date 8/9/2025
- MoPH Announces the Results of a Quality Control Test for Food Supplements
- Nassereddine Sponsors the Opening of the Annual Conference of the Lebanese Order of Physiotherapists
- Nassereddine Sponsors the Opening of the Annual Conference of the Lebanese Order of Physiotherapists
- Four Martyrs and 17 Wounded, including Four children, in the Total Toll of the Enemy's Attacks Yesterday
- Nassereddine Receives the Ambassadors of Brazil and Belgium
- Nassereddine Launches "Carol" Initiative to Implement Safety Standards in Nurseries
- Launching the National Strategy for Digital Transformation in the Health Sector 2025-2030
- Guidelines
- General Information on Private Daycares Regulation in Lebanon
- Information for Parents on Private Daycares in Lebanon
- Nassereddine Visits Two Adult Patients Who Underwent Kidney Transplants for the First Time with Full Coverage
- Nassereddine at the "Medical Expatriate" Conference
- Nassereddine Visits Two Pharmaceutical Factories in Dbayeh and Zikrit
- Cessation Clinics
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1411/1 , 1413/1 , 1416/1 & 1418/1 Date 13/8/2025
- Awareness Campaign on Smuggled and Counterfeit Medicines 2025
- Nassereddine Sponsors a Free Health Activity in Arab Salim
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1352/1 , 1353/1, 1354/1 & 1355/1 Date 7/8/2025
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1184/1 & 1188/1 Date 10/7/2025
- MoPH Announces a Comprehensive Survey of Food Supplements and Nutritional Products in Lebanon
- The Ministers of Health and Economy Discuss,Including Palliative Care in Insurance Policies
- Nassereddine Visits a Child Who Underwent a Kidney Transplant for the First Time with Full Coverage
- Launching of the "National Campaign to Awareness-Raising Drowning Prevention"
- General Preventive Measures and Preparation for Heat Waves
- Press Release from the MoPH on Snakebites and Antivenom in Lebanon
- Nassereddine Launched the Annual Report on Maternal Mortality
- Minister of Health from Hermel: Lebanon is not hostage, and let us be the owners of a comprehensive national decision.
- Climate Impacts Are Reshaping Public Health in Lebanon
- Nassereddine Receives the Chinese Ambassador
- The Ministries of Public Health and Information Launch an Awareness Campaign on Smuggled & Counterfeit Drugs
- Minister Nassereddine's Decision to Close a Beauty Center
- Nassereddine Inaugurates a Scientific Conference at Makassed General Hospital
- Delegation from the Syndicate of Press Photographers Visits Nassereddine and Explains their Suffering
- Nassereddine Inaugurates the Rehabilitation of the Dialysis Unit at Hariri Hospital, as an Initiative by "Beirut is Fine"
- Nassereddine Follows up on Projects to Establish and Develop Governmental Hospitals at the CDR
- Nassereddine Inspects Hospitals in Nabatieh and Hasbaya
- Nassereddine Sponsors an Awareness Campaign on Chronic Kidney Disease at KMC
- Nassereddine Represents the President of the Republic at ILMA Conference
- Nassereddine and the WHO Regional Director Inspecte the Healthcare Centers in the Suburb
- President Aoun Meet a Delegation from the WHO and Praise the Cooperation between Lebanon and the Organization
- Nassereddine Signs the 2026-2029 Cooperation Strategy with the WHO
- Nassereddine at the Graduation of Students from the Faculty of Medical Sciences at the Lebanese University
- Rabies Prevention
- Nassereddine Inaugurates Specialized Mobile Clinics Launched by Order of Malta
- Nassereddine and the Swiss Ambassador Discuss Activating Cooperation in Health Projects
- Nassereddine Inspects the Pharmaline Factory and Learns about the Latest Technologies Used in Drug Manufacturing
- Nassereddine Sponsors the Opening of the UBSA PHARMA Factory in Hraiche, Koura
- Nassereddine at the ASCO 2025 Cancer Conference at the American University
- Nassereddine Inaugurates the Medical Forum at the LU and Confirms Coordination in the Central Laboratory Project
- MoPH: There is no Problem with the Availability of Licensed Medicines
- Nassereddine Receives the New Iraqi Ambassador
- Nassereddine Distribute Certificates of Good Storage and Distribution of Medicines and Pharmaceutical Products
- Nassereddine discuss with a Delegation from the IsDB the Equipping of Governmental Hospitals
- Nassereddine Chair a Meeting of the Guarantor Parties
- Meeting at MoPH with International Partners Presentes a Roadmap for Health System Reforms
- Nassereldine and Al-Sulaiti Inspecte the New Building of Karantina Hospital
- National Pharmacovigilance Program Newsletter - Issue 15 -July 2025
- National Pharmacovigilance Program Newsletter-Issue 14 ِApril 2025
- Applications for Positions Advertised in Public Institutions
- Nassereldine Announces the Nomination of Miss Lebanon, Nada Kousa, as an Ambassador for the Mental Health
- Laws and Regulations
- Laws and Regulations
- Meeting of Representatives of Donor Countries and Entities at the Ministry of Public Health
- Nassereldine Representes the President of the Republic in a Condolence Visit to the Iranian Embassy
- National Mental Health Strategy 2024-2030
- The Ministry of Public Health Launches the “The Good Pharmacovigilance Practices Guideline”
- Advancing Cancer Treatment: From Chemotherapy to Precision Medicine
- Nassereldine Closes a Beauty Center that Did not Meet Legal Requirements
- Nassereldine Visites Mashmoushi and Agreed to begin Appointment Procedures
- Request for Procurement and Installation of PICU and NICU
- Request for Procurement and Installation of Radiology Equipment
- Request for Procurement and Installation of Medical Furniture
- Request for Procurement of MRI and PetScan
- Request for Procurement and Installation of Laboratory & Sterilization Equipment
- Request for Procurement and Installation of Computed Tomography Machine (CT Scan 64 Slices)
- Nassereldine Receives a Certificate of Appreciation from the Gavi Vaccine Alliance
- Nassereldine Representing the President of the Republic at the GAVI Summit
- Meeting on Sustainability, Environmental, and Social Governance at MoPH
- WHO Recommendations in case of a Nuclear Radiation Accident
- Nassereldine from Chtaura Hospital: We are Proud of this Hospital
- Nassereldine Toures Rayak Hospital
- Nassereldine Toures Salloum Medical Center
- Nassereldine Inaugurates the Medical Center's Conference on Advanced Nursing Services
- Nassereldine Toures Baalbek: We Affirm our Commitment to Supporting Governmental Hospitals
- Request for Procurement of Medical Equipment
- Al-Makassed Hospital Celebrates the Graduation of 16 Doctors from the College of Nursing
- Launching of the Project to Strengthen Governmental Hospital Systems,Blood Banks and the Central Warehouse
- MoPH Launches the Pandemic Response Fund Project in Partnership with the WHO
- MoPH Distribute Equipment for Emergency Preparedness to Governmental Hospitals
- Announcement about the Food Supplement
- Nassereldine Discusses with the National Mental Health Program and Embrace Ways to Promote Mental Health
- Advancing Cancer Treatment: From Chemotherapy to Precision Medicine
- Advancing Cancer Treatment: From Chemotherapy to Precision Medicine
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 947/1, 951/1 & 954/1 Date 11/6/2025
- Nassereldine Receives a Delegation from the General Labor Union
- Nassereldine Launches the Second Phase of Enhancing Children's Healthcare
- Lighting the Grand Serail in Solidarity with MS Patients
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 753/1 Date 13/5/2025
- Environmental and Social Commitment Plan
- Meeting at MoPH Discuss Settling Outstanding Financial Issues between Governmental Hospitals and NSSF
- Nassereldine Represents the President Aoun in Receiving Ambulances from Belarus at the Airport
- Nassereldine Calls for Tracking Down those Involved in the Islamic Hospital Incident
- MoPH Calls for a Tender to Purchase Specialized Medical Equipment for Governmental Hospitals
- Nassereldine at the ECIL Center for Early Intervention
- Nassereldine Launches an Initiative to Integrate Type 1 Diabetes Care into PHC Centers
- Open Invitation Call for Collaboration with ALMA
- Nassereldine Represents the President of the Republic at the Opening of the Order Of Pharmacists Conference
- Nassereldine Opens the Ophthalmologists' Conference
- Field Visit to Mersaco Pharmaceutical Warehouse
- Highlights of Minister Nassereldine 's Statements to the Newsmaker Program on RT
- Request for Procurement and Installation of Pediatric Intensive Care Unit (PICU) and Neonatal Intensive Care Unit (NICU)
- Request for Procurement of Magnetic Resonance Imaging (MRI) & Positron Emission Tomography (PET) scan
- Nassereldine Visits Hariri Hospital Accompanied by an Emirati Delegation to Inspect its Conditions
- UNHCR Informs Nassereldine that Hospitalization Coverage for the Displaced will be Suspended in November
- Awareness Workshop on the Dangers of Smoking at the Lebanese Order of Physicians
- Nassereldine Sponsores the Opening Ceremony of the Outpatient Department at Shifaa Specialty Hospital
- Living with Multiple Sclerosis: Innovations, Challenges, and Regional Perspectives
- Lebanon Regaines its Voting Rights in the World Health Organization
- Instructions from the Ministry of Health to Pilgrims
- Instructions from the Ministry of Health to Pilgrims
- Nassereldine : To Strengthen the Commitment to Prioritizing Care for Non-Communicable Diseases, Especially Cancer
- Morbidity
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 753/1 Date 13/5/2025
- Nassereldine Meets in Geneva with the Health Ministers of Iraq, Qatar, Syria and Monaco
- REAYA Programe
- Nassereldine Continues his Meetings in Geneva to Support the Lebanese Health System
- Life Expectancy and Mortality
- Risk Factors
- Field Visit to Pharmaline Pharmaceutical Factory
- The Ministry of Public Health Launches the Second Phase of "REAYA" Program
- Nassereldine Meets with the French Minister of Health in Geneva, affirming the Support for the Health System
- Follow-up Visit to Union Healthcare on the Implementation of MediTrack
- Nassereldine : Initial Support for Hariri Hospital and Positive Cooperation are Essential for Desired Renaissance
- The Director of Rafik Hariri Hospital Thanks the Minister of Public Health for his Inspection Visit
- Nassereldine Meets Rabab Al-Sadr and Discusses Ways of Cooperation with a Delegation from the Qatar Red Crescent
- Medical Supplies Donated by Brazil, and the Minister of Health Discusses Norway's Support for the Turkish Hospital
- Clarification from the Ministry of Public Health Regarding Meningitis and Neisseria Meningitidis
- New Hospitals Join the MediTrack System
- Trauma in Medicine Medical Conference at Beirut Arab University
- New Pharmacies Join the MediTrack System
- Living with Multiple Sclerosis: Innovations, Challenges, and Regional Perspectives
- Living with Multiple Sclerosis: Innovations, Challenges, and Regional Perspectives
- Workshop Event on the Regulation of Food Supplements in Lebanon
- Invitation to Pharmaceutical Institutions to Join MediTrack System
- Announcement of Training Courses on the MediTrack System
- MediTrack to Include New Types of Medicines and Diseases, Abiad
- Abiad and the Importing Companies Brought Up Challenges They Face in the Implementation of Meditrack
- Minister Abiad Officially Launches the Tracking System for Cancer Medicines
- Field Visit to Algorithm Pharmaceutical Factory
- Statement from MoPH Regarding the Death of a Child in a Nursery in Keserwan District
- Nassereldine Receives the Ambassador of the Sultanate of Oman
- Nassereldine Launches the National Awareness Campaign about Trans Fats in Cooperation with the American University
- Local Manufacturing Industries
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 543/1 Date 22/4/2025
- Nassereldine Participates in the Saeed Association's Awareness Activity against Colon Cancer
- The Ministry of Public Health and UNICEF launch a Policy to Protect Children in Nurseries in Lebanon
- Nassereldine: We are Working on Expanding Protocols and Introducing New Medications and the Cervical Vaccine
- Launching Ceremony of Tobacco Control Investment Case Study in Lebanon: 24 March 2025
- Guidelines from the Service of Preventive Medicine at the Ministry of Public Health during Sandstorm
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 502/1 Date 15/4/2025
- Nassereldine Visits the Maronite Patriarch, Cardinal Mar Bechara Boutros Al-Rahi, and Checks on his Health
- Opening of Azhar Al-Bekaa Dispensary under the Patronage of the Minister of Public Health Dr. Rakan Nassereldine
- Recent Israeli Attacks
- Where Can You Report your Adverse Drug Reactions or Adverse Events Following Immunization
- Nassereldine Condemns Attacks on Pharmacies
- The Ministry of Public Health Condemns the Attack on Rayak Hospital
- The Ministry of Public Health Receives 36 Tons of Iraqi Medical Aid
- The Ministry of Public Health Receives 40 Tons of Supplies from the European Union and UNICEF
- Nassereldine Announce of a Receipt of a Donation of Kidney Dialysis Supplies from the WHO
- HPV and Cervical Cancer: Advances in Prevention and Management
- Nassereldine Discusses with a Delegation from the World Bank the Completion of Joint Projects
- Request for Expressions oF Interest Consulting Services for Reaya Pilot Project Evaluation
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 397/1 Date 2/4/2025
- The Ministry of Public Health Condemns the Targeting of Ambulances in Naqoura
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 327/1 Date 13/3/2025
- Request for Bids for Procurement and Installation of CT Scan Multi Slices
- Influenza Surveillance
- Issuance of the List of Pharmacies Connected to "Meditrack System"
- Ministers of Education and Health Announce the Medical Examination Program for Public School Students
- The Inauguration of the Ircad Liban Academy under the Patronage of President Aoun
- Contact us
- Launching an Economic Feasibility Study on Tobacco Control
- Nassereldine: Investing in the Public Health Sector is Necessity that Requires Everyone's Cooperation
- HPV and Cervical Cancer: Advances in Prevention and Management
- Nassereldine Review the Conditions of Al-Hariri Hospital
- The Ministry of Public Health Condemns the Attack on Halba Hospital
- MoPH: Seven Martyrs and Fifty-Two Wounded on the Lebanese-Syrian Border
- Seven Martyrs and Forty Wounded in Israeli Raids on Lebanese Areas Today
- World TB Day- 2025
- Nassereldine Follows up on Governmental Hospitals Development Projects at the CDR
- Nassereldine and UNICEF Launche the Assistance and Care for War-Wounded and Affected Children (ACWA)
- NCD Toolkit Videos
- Nassereddine Reviews the Conditions of Deir al-Qamar Hospital and Receives the Syndicate of Hospitals
- The Role of Telehealth in Overcoming Healthcare Access Barriers
- Nassereldine Held a Meeting with the World Bank Mission
- Nassereldine Met with the Egyptian Ambassador and Discussed Bilateral Cooperation with a Delegation from the EU
- Updated List of Pharmacies Connected to "Meditrack System"
- Nassereldine Concludes his Southern Tour at Tebnin Governmental Hospital
- Nassereldine at Salah Ghandour Hospital: To Work on Enhancing Confidence and Securing People’s Health Needs
- Nassereldine at Bint Jbeil Hospital, which is Gradually Returning to Work
- Nassereldine Begins a Tour in the South from Mays Al-Jabal Hospital
- Seminar at the French Cultural Center in Beirut on Strengthening the Health Sector in Times of Crises
- Minister Nassereldine Closes Nurseries Tomorrow in Mountainous Areas
- Nassereldine Explains the Mechanism for Obtaining Vaccination Certificate Cards for the Upcoming Hajj Season
- Nassereldine Discusses Joint Projects with the French Ambassador and the WHO Representative
- 4Ws
- National AIDS Control Program in Lebanon
- National Tuberculosis Program
- A New Method for Reporting Side Effects of Medications and Vaccines through the Vigimobile App
- The Ministry of Public Health
- Request for IT Officer
- Statement of Condemnation from MoPH Regarding the Kidnapping of Islamic Risala Scout Paramedics in Houla
- Request for Expression of Interest of External Financial Audit
- Abiad Handed Over the Ministry of Health to his Successor and Listed its Achievements
- The Role of Telehealth in Overcoming Healthcare Access Barriers
- Two Year Review of the National Health Strategy: Vision 2030
- Lebanon National Health Strategy-Vision 2030
- The Role of Telehealth in Overcoming Healthcare Access Barriers
- Issuance of Minister's Decision No.264-2025 Regarding the Work of Pharmaceutical Institutions on MediTrack
- Abiad: Cancer Medicine Stock is Sufficient for at Least Five Months
- Emerging from Crisis Lessons Learned from Lebanon’s Recent Emergency Response
- Abiad Presents a Project to Support Kidney Dialysis Departments in 20 Governmental Hospitals
- Abiad Receives Aid from Rotary Clubs in Cyprus and Beirut for PHC Centers
- MoPH Issues updated Cumulative Report on Enemy Attacks on Health Sector
- IOM and Partners Launch Project to Strengthen Environmental Health Awareness in Lebanon
- Abiad from the Turkish Hospital : I Fulfilled the Promise to Operate it as a Service to our People and our Community
- Healing the Healers – Supporting Yourself and Your Patients in the Aftermath of Conflict
- MoPH Announces Delivery of more than Three Million Medicine Boxes to Displaced Persons during Israeli Aggression
- Cooperation between the Ministry of Public Health and EMTs during the War
- National Pharmacovigilance Program Newsletter-Issue 13 January 2025
- National Pharmacovigilance Program Newsletter-Issue 12 October 2024
- Final Result of the Israeli Enemy’s Attacks Yesterday
- Ministry of Public Health's Partnership with Middle East Airlines during the Last War
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 175/1 & 181/1 & 182/1 Date 22/1/2025
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 38/1 & 39/1 & 40/1 Date 2/1/2025
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 97/1 Date 14/1/2025
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 1367/1 Date 25/9/2024, 1467/1 & 1468/1 Date 22/10/2024, 1662/1 & 1663/1 Date 20/11/2024
- MoPH Publishes the Fourth Schedule of Aid Distributed to Hospitals and Emergency Societies
- Request for Pharmacist
- Abiad Visits the Turkish Hospital, Concluding his Tour in the South and Nabatieh
- Abiad: We Are Committed to Providing the Best Health Services to Ctizens, Especially in the Affected Areas
- Abiad Begin his Southern Tour at Marjeyoun Hospital
- Abiad and the Spanish Foreign Minister on an Inspection Tour of Baabda Governmental Hospital
- Roads for Life Honors the Nursing Sector in Governmental Hospitals under the Patronage of the MoPH
- Emerging From Crisis: Lessons Learned From Lebanon’s Recent Emergency Response
- Statistics on Private Daycares in Lebanon
- Abiad Discuss with Pharmacists Compensation and the Mechanism for Returning Demolished Pharmacies to Work
- Acute Flaccid Paralysis
- Mikati Sponsor the Opening of the Cardiac Catheterization and Dialysis Department at Tripoli Governmental Hospital
- Abiad Discuss in Paris the Rehabilitation of the Central Laboratory after Securing Funding
- 52,500 Medicine Boxes for Displaced People Due to the Syrian Events
- Abiad Participates in the Opening of the WHO Academy in the Presence of Macron
- Request for Consultancy Services for Warehouse Pharmacist
- Abiad Holds Meetings to Coordinate Aid for Displaced People as a Result of the Syrian Events
- Abiad Delivers Lebanon's Speech at the Council of Arab Health Ministers in Baghdad
- MoPH Confirms Monitoring the Conditions of Lebanese and Displaced Syrians who Took Refuge in Lebanon
- Request for Pharmacist and IT Officer for MoPH
- Abiad Tours the Hospital Sector in the Suburb and Stressed the Need for Reconstruction
- Abiad Receives a Donation of Medical Equipment for Children’s Care from the Czech Republic
- The Ministry of Public Health Closes a Clinic in Al-Bireh
- Abiad Continues his Tour of the Hospitals in the South and Nabatieh and Inspects Tebnin Hospital
- Abiad Inspectes Nabih Berri Governmental Hospital and Sheikh Ragheb Harb Hospital in Nabatieh
- Abiad Inspects Jabal Amel Hospital
- Abiad at the End of a Tour of Baalbek Hospitals: Solidarity Failed the Israeli War on Lebanon
- Abiad Tours Hospitals in the Northern and Central Bekaa and Baalbek-Hermel
- Humanitarian Crises Responses
- 4,047 Martyrs and 16,638 Wounded, the Total Updated Toll of the Israeli Aggression
- MoPH,UNICEF and WHO, Launche the First Report in the Region on Child Development and Prevention Guidelines
- Measles
- Meningococcal Infection
- Meningitis
- World's AIDS Day 2024
- MoPH Notes the Resilience of the Health System and Thanks the Workers Who Did not Spare their Lives
- 3,961 Martyrs & 16,520 Wounded since the Start of the Aggression, and the Toll on Tuesday was 78 Martyrs & 266 Wounded
- MoPH Publishes the Third Schedule of Aid Distributed to Hospitals and Emergency Societies
- Free Medicines Distributed by the Ministry of Public Health
- List of Medications Provided By MoPH in the Catastrophic Disease Management Program
- Cumulative Report on the Support Provided to Displaced Citizens
- 3,823 Martyrs and 15,859 Wounded since the Start of the Aggression, and Yesterday’s Toll was 55 Martyrs and 160 Wounded
- 3,768 Martyrs and 15,699 Wounded since the Start of the Aggression, and Yesterday’s Toll was 14 Martyrs and 73 Wounded
- The 19th Qatari Aid Plane Arrives to Beirut
- Self-care
- Self-Help+ Podcast
- 4Ws Online Platform
- Step by Step
- DRAFT National Mental Health Strategy 2023-2030- FOR PUBLIC REVIEW
- 3,754 Martyrs and 15,626 Wounded since the Start of the Aggression, and Yesterday’s Toll was 84 Martyrs and 213 Wounded
- 3,670 Martyrs and 15,413 Wounded since the Start of the Aggression, and Yesterday’s Toll was 25 Martyrs and 58 Wounded
- MoPH: Two Paramedics were Martyred and Four were Wounded because they were Pursued by Israeli Marches
- MoPH Mourns Alam: He was Known for his Closeness to People and He's a Great Loss
- Cumulative Report on the Support Provided to Displaced Citizens
- 3,645 Martyrs and 15,355 Wounded since the Start of the Aggression, and Yesterday’s Toll was 62 Martyrs and 111 Wounded
- The National Vaccination Campaign against Polio, Measles, Rubella and Abu Kaab Diseases
- 3,583 Martyrs and 15,244 Wounded since the Start of the Aggression, and Yesterday’s Toll was 25 Martyrs and 121 Wounded
- MoPH is Working Hard to Receive and Distribute Medical and Humanitarian Aid
- A Paramedic was Killed and Three Wounded in Kfardounine
- Abiad Launches the National Influenza Vaccination Campaign
- 3,558 Martyrs and 15,123 Wounded since the Start of the Aggression, and Yesterday’s Toll was 14 Martyrs and 87 Wounded
- Abiad Launches the National Vaccination Campaign against Infectious Diseases in Cooperation with UNICEF and WHO
- 3,544 Martyrs and 15,036 Wounded since the Start of the Aggression, and Yesterday’s Toll was 28 Martyrs and 107 Wounded
- Community Awareness- PHEOC
- Cumulative Report on the Support Provided to Displaced Citizens
- 3,516 Martyrs and 14,929 Wounded since the Start of the Aggression, and Yesterday’s Toll was 35 Martyrs and 143 Wounded
- Two Paramedic Martyrs in Qana
- Abiad Launches an Unprecedented Emergency Health Care Coverage Program
- Two Paramedics Were Killed and Two Wounded in Three Israeli Attacks in Southern Lebanon
- 3,481 Martyrs and 14,786 Wounded since the Start of the Aggression, and Yesterday’s Toll was 29 Martyrs and 122 Wounded
- 3,452 Martyrs and 14,664 Wounded since the Start of the Aggression, and Yesterday’s Toll was 7 Martyrs and 65 Wounded
- MoPH: Two Additional Barbaric Attacks on Paramedics in Burj Rahal and Kfar Tebnit
- 3,445 Martyrs and 14,599 Wounded since the Start of the Aggression, and Yesterday’s Toll was 59 Martyrs and 182 Wounded
- Cumulative Report on the Support Provided to Displaced Citizens
- MoPH Denounces the Continued Unchecked Violence in the Enemy's Raid on the Civil Defense Center in Douris
- 3,386 Martyrs and 14,417 Wounded since the Start of the Aggression, and Yesterday’s Toll was 21 Martyrs and 73 Wounded
- Resources
- Help Seeking
- 3,365 Martyrs and 14,344 Wounded since the Start of the Aggression, and Yesterday’s Toll was 78 Martyrs and 122 Wounded
- Videos
- Syrian Crisis
- Suicide
- Substance Use
- Step-by-Step (SBS)
- Response to National Emergencies (i.e. Beirut Blast, COVID-19, etc.)
- Research and Publications
- Psychotropic Medications
- Newsletters
- National Strategy and Related Documents
- 3,287 Martyrs and 14,222 Wounded since the Start of the Aggression, and Yesterday’s Toll was 44 Martyrs and 88 Wounded
- Abed
- MoPH Publishes the Distributing Medicines to PHC Centers that Provide Services to Displaced People
- Mental Health Professionals
- National HIV Strategic Plan 2023-2028
- Cumulative Report on the Support Provided to Displaced Citizens
- 3,243 Martyrs and 14,134 Wounded since the Start of the Aggression, and Yesterday’s Toll Was 54 Martyrs and 56 Wounded
- 3,189 Martyrs and 14,078 Wounded since the Start of the Aggression, and Yesterday’s Toll Was 53 Martyrs and 99 Wounded
- 3,136 Martyrs and 13,979 Wounded since the Start of the Aggression, and Yesterday’s Toll was 19 Martyrs and 91 Wounded.
- MoPH Publishes the Third Schedule for Distributing Medicines to PHCs that Provide Services to Displaced People
- MoPH Publishes the Second Schedule of Aid distributed to 71 Governmental and Private Hospitals and First Aid Associations
- 3,117 Martyrs and 13,888 Wounded since the Start of the Aggression, and yYesterday’s Toll Was 15 Martyrs and 69 Wounded.
- Issuance of Drugs Public Price List Updated on 11/11/2024 in Implementation of Resolution 1559/1
- Issuance of Drugs Public Price List Updated on 11/11/2024 in Implementation of Resolution 1559/1
- Mental Health Diploma
- How Do Displaced Citizens Access Chemotherapy?
- Issuance of Minister's Decision No.1559/1 of 11/11/2024 Regarding the Cancellation of Resolution No.945/1
- Mental Health Conditions - Awareness
- Mental Health Campaigns – National
- Laws and Regulations
- Guiding Documents for Capacity Building
- Mental Health Campaigns – National
- MoPH Allocates an Exceptional Financial Ceiling to Support Charity Hospital
- 3,102 Martyrs and 13,819 Wounded since the Start of the Aggression, and Yesterday’s Toll was 52 Martyrs and 161 Wounded
- Cumulative Report on the Support Provided to Displaced Citizens
- Cumulative Report on the Support Provided to Displaced Citizens
- Abiad: The Proactive Plan for the Crisis Has Proven Effective
- 3,050 Martyrs and 13,658 Wounded since the Start of the Aggression, and Yesterday’s Toll Was 37 Martyrs and 105 Wounded
- Mechanism of Distributing Medications for Catastrophic Diseases through Pharmacies
- Lebanese National Pharmacovigilance Program Scientific Publications
- 3,013 Martyrs and 13,553 Wounded since the Start of the Aggression, and Yesterday’s Toll was 11 Martyrs and 61 Wounded
- Abiad Visits the Burns Department in Geitaoui Hospital, Accompanied by Riza and Abu Bakr
- Technical Assistance To The Administrative Simplification Project
- Japanese Emergency Grant Aid
- Emergency Response Medical Team
- 3,002 Martyrs and 13,492 Wounded since the Start of the Aggression, and Yesterday’s Toll was 16 Martyrs and 90 Wounded
- Abiad Announces the Start of Work in New Departments in the Turkish Hospital
- Elderly Centers
- Primary Health Care
- MoPH Deplores the Martyrdom of Two Paramedics and the Damage to Tibnin and Baalbek Governmental Hospitals
- 2,968 Martyrs and 13,319 Wounded since the Start of the Aggression, and Yesterday’s Toll was 71 Martyrs and 169 Wounded
- 2,986 Martyrs and 13,402 Wounded since the Start of the Aggression, and Yesterday’s Toll was 18 Martyrs and 83 Wounded
- Abiad after his Tour in the North:Our Responsibility is to Listen to the Various Forces to Identify the Gaps
- 2,897 Martyrs and 13,150 Wounded since the Start of the Aggression, and Yesterday’s Toll Was 30 Martyrs and 103 Wounded
- List of Aids sent by Expatriates: Solidarity with Lebanon Achieves Steadfastness
- 2,867 Martyrs and 13,047 Wounded since the Start of the Aggression, and Yesterday’s Toll Was 45 Martyrs and 110 Wounded
- Cumulative Report on the Support Provided to Displaced Citizens-31-10-2024
- In Two Additional Incidents Today, Four Paramedics were Martyred in Dardaghia and a Vehicle Burned in Selaa
- For the Second Time Today One Paramedics Killed and Two Wounded in Deir Al-Zahrani
- Paramedic Killed and Two Wounded in an Israeli Enemy Raid on an Ambulance in Zefta
- Paramedic Killed and Two Wounded in an Israeli Enemy Raid on an Ambulance in Zefta
- 2,822 Martyrs and 12,937 Wounded since the Start of the Aggression, and Yesterday’s Toll Was 30 Martyrs and 165 Wounded
- Abiad Concludes his Tour in Iqlim Al-Kharroub Noting the Solidarity Shown by the Lebanese in Light of this Crisis
- Abiad Tours PHC and Shelter Centers in Iqlim Al-Kharroub
- 2,792 Martyrs and 12,772 Wounded since the Start of the Aggression, and Yesterday’s Toll was 82 Martyrs and 180 Wounded
- MoPH Publishes Detailed List for Distributing Medicines to PHC centers that Provide Services to Displaced People
- 2,710 Martyrs and 12,592 Wounded since the Start of the Aggression, and Yesterday’s Toll was 38 Martyrs and 124 Wounded
- Cumulative Report on the Support Provided to Displaced Citizens- 28/10/2024
- Abiad Submits a Report Documenting 55 Enemy Attacks on Hospitals and 201 on Emergency Services
- Abiad Receives an Emirati Aid Ship: We Appreciate the UAE’s Support for Lebanon’s Position Seeking a Ceasefire
- Abiad Receives the First Batch of Indian Medical Aid Amounting to 33 Tons
- Cumulative Report on the Support Provided to Displaced Citizens- 24/10/2024
- Detailed List of Medical Aids Distribution
- MoPH Denounces the Attack on Two of Lebanon’s Largest Hospitals
- Additional Medical Aid Arrives at Rafic Hariri International Airport
- Cumulative Report on the Support Provided to Displaced Citizens
- Abiad Receives a Shipment of Medical Aid from China: a Message of Solidarity to the Lebanese and Financial Support to Hospitals
- MoPH Denies News of the Evacuation of Baalbek Governmental Hospital
- Cholera in Lebanon
- Abiad Assures that the Issue of Medicine is Under Control and MoPH is on High Alert for Cholera
- Cumulative Report on the Support Provided to Displaced Citizens
- Statement
- Daily Cumulative Report on the Support Provided to PHC Centres to Displaced Citizens
- A Joint Press Conference by Ministers Abiad and Yassin to Clarify the Aid Mechanism
- Abiad Discuss with the Parliamentary Health Committee the Update on the Emergency Plan
- Detailed List of the Aid Distributed to Hospitals and Emergency Services
- A New Batch of Qatari Aid Arrives
- Clinical Management of Rape
- MoPH Extends Work With Approvals on Aman Platform
- Al-Khater Toures with Abiad and Yassin at Karantina Hospital
- Al-Khater Announces an Air Bridge of Aid
- Abiad Receives Aid and Medical Supplies Provided by France in Cooperation with Qatar
- ATLAS
- Abiad Presentes the Mechanism for Receiving and Distributing Medical Aid
- MoPH: There is no Evidence so far of the Use of Uranium in Israeli Attacks against Lebanon
- An Additional Massacre and War Crime in Baraashit: Ten Firefighters Were Martyred in an Initial Toll
- Abiad ReceiveS 25 Tons of Medicines and Medical Supplies from UNICEF, Funded by the British Government
- An Egyptian Plane Loaded with Medical and Humanitarian Aid Arrives at the Airport
- Abiad Receives Forty Tons of Aid, Medicines and Medical Supplies Provided by the UAE
- Abiad Receives at the Airport a Shipment of International Medicines and Medical Supplies
- Abiad Presentes a New Total of Attacks on the Health Sector
- The Ministry of Public Health Requests to Contract with Fifteen Controller Doctors
- MoPH Reminds about the Medical Services Provided to the Displaced and Adds 1214 to the Hotline 1787 to Communicate with Them
- MoPH Mourns 6 Martyrs of Paramedics in Sohmor in the Western Bekaa
- MoPH Reminds us of the Medical Services Provided to the Displaced and Adds 1214 to the Hotline 1787
- Abiad Detailes the Medical Facilities Provided to the Displaced and Ensuring Communication on 1214 and 1787
- Abiad Meets with the French Foreign Minister and Received a Donation of Aid for Emergency Treatment
- MoPH Denounces the Series of Targeting of Paramedics
- MoPH Calls on Hospitals in Beirut and the Regions to be Ready to Evacuate the Suburb’s Hospitals
- Abiad and Bakhash Launche the Initiative of Specialized Clinics for Long-term Treatment of the Wounded
- Abiad Detailes the Medical Facilities Provided to the Displaced and Ensuring Communication on 1214 and 1787
- MoPH Confirms the Continues Closure of Nurseries in Places Exposed to Aggression
- Abiad Explaines the Details of the Medical Care Provides to the Displaced
- The Order of Nurses Announces a Volunteer Campaign under the Title “Strengthening the Nursing Staff”
- Request for Quotation for Procurement of Chiller System for the Turkish Hospital in Saida
- Request for Quotation for Procurement of Power Generator for the Turkish Hospital in Saida
- Closure of Nurseries until the End of the Week in all Lebanese Territories
- Abiad: “We Have a Difficult Stage Ahead of Us, and We Remain on the Front Lines Alongside our Society.”
- 1564, The Lifeline
- MHPSS Task Force Minutes of Meetings
- Closure of Nurseries Tomorrow across all Lebanese Territories
- MoPH Reminds that Foreign Doctors must Obtain Prior Permission in Accordance with the Laws
- The Ministry of Health Receives a Shipment of Iraqi Aid
- Seventy Martyrs, the Total Toll for Three Days of Successive Israeli Attacks
- MoPH Requests that Cold Operations be Stopped to Make Room for Receiving the Wounded
- Abiad Praises Fruitful Cooperation, and Al-Khalil: We are Mobilized in These Difficult Circumstances
- Abiad at the Lebanese Order of Physicians: The Mechanism for Paying Health Sector Dues will Begin Next Week
- MoPH: Blood Banks are Equipped with Units and There is no Need for Donation Campaigns at the Present Time
- Abiad Concludes his Bekaa Tour, Praising the Efforts of the Hospital Teams: All Care is Provided to our Wounded
- Abiad in Rayak Hospital: We stand by the Injured in their Future Treatment
- Minister Abiad Inspectes the Injured in Baalbek Hospitals
- Abiad Stresses the Restoration of Readiness in the Face of a Treacherous Enemy
- Abiad Presentes a Total of the Two Days of the Hostile Security Breach: 37 Martyrs and 2931 Wounded
- Mikati Receives a Solidarity Call from Erdogan and Inspected the Health Emergency Center- 18/9/2024
- Abiad in a Second Tour of Hospitals
- Abiad: Our Public and Private Health System Responded with Dedication and Responsibility
- MoPH Announces the Activation of the Hotline 1214 for Reviews about Cancer and Incurable Diseases Medications
- Abiad Inspectes the Wounded in the Capital and Suburb Hospitals
- MoPH Denies Inaccurate Statistical Information
- Abiad in an Emergency Press Conference: The Initial Toll of the Security Incident is 9 Martyrs and about 2800 Wounded
- Second Urgent Statement Issued by the Ministry of Public Health
- MoPH Asks Hospitals to be on Maximum Alert to Receive the Number of Injured People Arriving at Them
- MoPH Confirms the Continuation of Its Proactive Campaign to Vaccinate against Cholera
- Laying the Foundation Stone for the New Building of Beirut Governmental University Hospital with Qatari Support
- AIMS
- 2024 MHPSS TF Minutes of Meeting
- Abiad Launches the First Phase of “Reaya” Program
- Abiad Receives 33 Tons of Essential Medical Supplies from UNICEF to Help Raise Readiness in Case the Aggression Expands
- Public Health Emergency Operation Center- PHEOC
- COVID-19 Vaccine
- Abiad Concludes his Tour in Minieh-Denniye and Follows up on the Epidemiological Issue
- Abiad Presentes the Extent of Human and Material Losses in the Health Sector Since the Beginning of the Israeli Aggression
- Six Injuries in an Update on the Toll of the Israeli Enemy Raid on the Town of Khirbet Silm
- Three Very Minor Injuries in the Israeli Enemy Raid on the Town of Khirbet Silm
- Three Martyrs and Two Wounded from the Lebanese Civil Defense in the Initial Toll of an Attack by the Israeli Enemy in the Town of Frun
- Two Civil Defense Personnel Injured in Qabrikha, and MoPH Reiterates its Condemnation of the Enemy’s Insistence on Attacking Health Teams
- Suffocation Due to the Enemy throwing Phosphorus on Kfar Kila
- Wounded and Suffocated Due to Israeli Artillery Shelling of Kfar Kila and Phosphorus on Burj Al-Muluk
- Four Wounded as a Result of the Israeli Enemy Raid on the Town of Hanin
- Abiad Inaugurates The Beirut Society Primary Care Center in Beit Fakas
- Abiad at Al-Iman Primary Care Center
- Abiad Continues his Tour in Dinniyeh and Visites the Governmental Hospital
- Abiad:Twenty Eight million Dollars budget Allocated to Support Care Centers
- A Martyr and a Wounded Person as a Result of the Israeli Enemy's Raid on the Town of Kafra
- Three Wounded as a Result of the Israeli Enemy Raid on the Town of Houla
- A Martyr and Two Wounded as a Result of the Israeli Enemy's Bombing of the Town of Qabrikha
- Four Wounded in Update on the Toll of the Israeli Enemy Raid on the Town of Markaba
- Two Wounded in Israeli Raid on Markaba Town
- Wounded in Israeli Targeting on Khiyam Road
- National Immunization Calendar
- MoPH Continues Campaign against Cholera and Calls on Citizens to Take the Vaccine
- Three Wounded in Israeli Raid on Markaba Town
- A Citizen Suffocated Due to the Enemy throwing Phosphorus on Al-Khayam
- Three Wounded in Israeli Raid on Beit Yahoun, Beit Lif Raid Death Toll Rises to One Martyr and Four Wounded
- The Number of Wounded in the Beit Lif Raid Rises to Eight
- One Martyr and Two Wounded in an Israeli Raid on the Town of Beit Lif
- Four Wounded in Israeli Enemy Raid on Aita al-Shaab Town
- Inauguration of a Project to Supply the Turkish Hospital with Solar Energy
- Two Martyrs in the Raid on Naqoura
- One of the Wounded in the Wadi al-Kafour Raid was Martyred, Bringing the Number of Martyrs to Eleven
- MoPH Condemns the Enemy's Insistence on Targeting Health Facilities Like what Happened in Blida Yesterday
- A Citizen Suffered from Suffocation Due to the Enemy throwing Phosphorus on Khiam
- Abiad: The Decisions to Increase Coverage will Make a Difference
- Wounded in the Raid on Baalbek
- Four Wounded this Morning, Three in the Enemy Raid on Al-Majadil and One Wounded in Sheheen
- A Citizen was Admitted to Intensive Care after Inhaling Phosphorus in Wazzani
- Abiad Inspects the Crisis Cell in Beirut Municipality
- MoPH Completes its Investigation into the Death of a Citizen after Spraying Pesticides in her Home
- Wounded in the Raid on Majdal Zun
- Two Martyrs in an Israeli Raid on the Town of Al-Tayri
- A Martyr in a Drone Attack in the Town of Khiam
- Two Wounded in Series of Israeli Raids on Southern Lebanon this Morning
- MoPH Launches a Vaccines Campaign against Cholera in Anticipation of its Renewed Spread
- MoPH Calls for not Attributing Information to the Ministry that Was not Issued by It
- Martyr in Preliminary Toll of Raid on Ma'arka Town
- Cumulative Emergency Report-13-8-2024
- Cumulative Emergency Report-20-8-2024
- Preliminary Toll of the Raid on the Abbasiya Town Junction
- Two Martyrs and Three Wounded in Mays al-Jabal and Aitaroun
- Three Martyrs in the Enemy Raid on Tyre Harfa
- Two Martyrs, Including a Child, in the Initial Toll of the Raid on Aita al-Jabal
- UNHCR Assures the Minister Abiad of Covering all Syrian War Wounded Known to Them
- Minister Abiad Concludes his Tour in the North
- Sheltering the Displaced and Ensuring their Health Services in the Meetings of Minister Abiad
- Abiad Visits Tripoli Governmental Hospital in Al-Qobba
- Abiad Inaugurates the Beirut Primary Care Association Center in Tripoli
- Final Toll of Bekaa Raids: One Martyr and Thirty Wounded
- Abiad Tours in the North, the Third within a Week, to Raise Readiness
- One Martyr in Initial Toll of Raid on Car in Sidon
- Two Lebanese and Syrian Martyrs in Beit Lif and Al-Wazzani this Morning
- Update on the Toll of the Raids on the Bekaa: One Martyr, Twenty Wounded, Including One in Critical Condition, and Eight Children
- Update on the Preliminary Toll of the Raids on the Bekaa: One Martyr and Nineteen Wounded
- Ten Wounded in Initial Toll of Raids on Bekaa
- Update on the Toll of the Israeli Raid on Al-Dhuhayrah: Four Martyrs and Two Wounded
- Update on the Toll of the Israeli Raid on Al-Dhuhayrah: Three Martyrs and Two Wounded
- MoPH Announces Four Injured, Including Three Paramedics, in Raid on Wadi Hamoul
- Two Martyrs in the Preliminary Toll of the Two Raids on Al-Dhaheira
- Abiad Met with the Crisis Cell in Sidon and Associations Concerned with Providing Services to the Displaced
- Syrian Wounded in the Bombing of Khiam
- Abiad Visits Ain Wzein Hospital and the PHC in Baakline
- Final Toll of Bekaa Raids: Eleven Wounded
- Eight Wounded in Initial Toll of Raids on Bekaa
- A Martyr in the Initial Toll of the Raid on Deir Qanoun Ras al-Ain - Tyre
- Update: The Number of Wounded in the Bekaa Raids Rises to nine, and the Number of Al-Mansouri Wounded to Two
- Palestinian Woman Injured in Raid on Al-Mansouri
- Three Citizens from Qabrikha are Being Treated in Hospital for Inhaling Phosphorus
- Citizen Admitted to the Hospital Due to Complications from Phosphorus Inhalation
- Two Martyrs in the Israeli Aggression on Houla
- Two Wounded in the Israeli Aggression on Aita al-Shaab
- Two Wounded in the Israeli Aggression on a House in Shebaa
- A Martyr and a Wounded Person in the Israeli Aggression on the Town of Shebaa
- Three Wounded in the Israeli Aggression on Markaba
- A Civilian Martyred in Motorcycle due to the Israeli Aggression in Tyre
- Second updated toll of the Israeli Aggression on Wadi al-Kfour
- Non Final Updated Toll of the Israeli Aggression on Wadi al-Kfour
- The Toll of the Israeli Aggression on Khiyam
- St George Hospital: The Injured in the Marjeyoun Raid are Being Treated at the Full Expense of MoPH
- MoPH Expresses Surprise at Misleading News about not Covering all War Wounded
- Statement on Monkeypox
- The Toll of the Israeli Aggression on Aitaroun
- The Toll of the Israeli Aggression on Marqaba
- Abiad Visits PHCs in the Iqlim al-Kharoub Region
- Abiad Inaugurates the Chemotherapy Department at Siblin Hospital Funded by the Qatar Red Crescent
- Updated Toll of the Israeli Aggression on Al-Khiam and Qabrikha
- The Toll of the Israeli Aggression on Qabrikha
- The Toll of the Israeli Aggression with Phosphorous Shells on Al-Khiam
- Updated Toll of the Israeli Aggression on Marjeyoun
- Abiad Visits Health Centers in Aley
- Initial Toll of the Israeli Aggression on Marjeyoun
- The Toll of the Israeli Aggression on Blida
- The Toll of the Israeli Aggression on Rab Tlatin
- Updated Toll of the Israeli Aggression on the Abbasiya Town Junction
- The Toll of the Israeli Aggression on Shihin
- The Toll of the Israeli Aggression on Bar'ashit
- The Toll of the Israeli Aggression on Kfar Kila
- Detailed Preliminary Toll of the Raid on Ma'aroub
- The Toll of the Israeli Aggression on the Town of Taybeh
- A Civilian Martyred Due to his Wounds
- The Toll of the Israeli Aggression on the Town of Wazzani
- Updated Toll of the Israeli Aggression on Majdal Selem
- Updated Toll of the Israeli Aggression on Majdal Selem
- Four Wounded in Two Enemy Raids on Majdal Selem
- The Toll of the Israeli Aggression on Majdal Selem
- Abiad Warns against Returning to Pre-Financial Crisis Practices
- The Toll of the Israeli Aggression with Phosphorous Shells on Kfar Kila
- The Toll of the Israeli Aggression on Sidon
- MoPH Condemns the Repeated Israeli Attacks on Ambulance Teams
- The Toll of the Israeli Aggression on Naqoura
- The Toll of the Israeli Aggression on the Town of Hanawiyeh
- Initial Toll of the Israeli Aggression on Yarin
- Open Meetings at the Ministry of Health to Increase Preparedness
- Abiad Chairs a Meeting of Iklim Al-Kharoub to Raise the Region's Readiness in Case the Aggression Expands
- Final Toll of the Israeli Aggression on Jawiya
- Updated Toll of the Israeli Aggression on Jawiya
- Initial Toll of the Israeli Aggression on Jawiya
- Initial Toll of the Israeli Aggression on Aitaroun
- The Outcome of the Israeli Aggression with Phosphorous Shells on Shebaa
- The Outcome of the Israeli Aggression on Shaqra
- The Toll of the Israeli Aggression on Adaisseh - Rab Al-Thalathin
- Updated Toll of the Israeli Aggression on Mefadoun and Wazzani
- Preliminary Results of the Israeli Aggression on Mefadoun and Khiyam
- The Outcome of the Israeli Aggression with Phosphorous Shells on Al-Khiam and Talousa
- Updated Toll of the Israeli Aggression on the Town of Aba
- Initial Toll of the Israeli Aggression on the Town of Aba
- The Outcome of the Israeli Aggression on Rab Tlatin
- The Outcome of the Israeli Aggression on Mays al-Jabal
- Updated Toll of the Israeli Aggression on Houla
- The Outcome of the Israeli Aggression on Houla
- The Outcome of the Israeli Aggression on Beit Lif
- Updated Toll of the Israeli Aggression on Deir Siryan
- The Outcome of the Israeli Aggression on Deir Siryan
- One Person was Injured in the Israeli Aggression on Tyre Harfa
- Final Toll of the Israeli Aggression on a Vehicle between Al-Bazouriyeh and Wadi Jilo
- MoPH: Seven Martyrs is the Final Toll of the Suburb Aggression
- UNICEF Distributes 65 Tons of Medicines and Medical Equipment in Collaboration with MoPH
- Abiad Receives Medical Aid from the WHO
- Health Emergency Center: Distributing Tons of Supplies and Medicines to Raise the Readiness of the Health Sector
- MoPH in an Updated Toll of the Attack on Shamaa: 4 Syrians Killed and 5 Wounded
- Initial Toll of the Shamaa Raid
- Abiad: We’re Raising the Preparedness of the Health Sector to Face any Possible Escalation
- Abiad: We Continue to Cover the War-Wounded
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 999/1 Date 30/7/2024
- Update from MoPH: The Number of Martyrs has Risen to 5
- Update from MoPH: The Number of Martyrs has Risen to 4
- Update from MoPH: 3 Martyrs, Including a Girl and a Boy, and 74 Wounded, and the Search Continues for Missing Persons
- MoPH: The Aggression on the Suburb Resulted in the Martyrdom of a Woman and the Injury of Sixty-Eight People
- Abiad Concludes his Bekaa Tour by Opening a Clinic in Saadnayel
- Abiad during his Bekaa Tour: We Pay Attention for the Remote and Distant Areas
- Preventive Health Care Directorate Rejects Indiscriminate Accusations and Calls for a Review of Laws
- Abiad and Bekaa Governor Discuss the Reopening of Bar Elias Hospital
- MoPH Launches Investigation to Determine Cause of Death of Woman who Sprayed Pesticides in her Home
- Abiad Inspects Batroun Hospital after the Collapse of Part of the Roof of the Dialysis Room
- Evaluation of the Lebanese-French Framework Agreement for Health Cooperation One Year after its Signing
- Request for Quotation for Procurement of Goods for the Turkish Hospital in Saida
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 859/1 & 862/1 & 874/1 & 875/1 & 877/1 Date 3/7/2024
- Mikati Participates with Abiad in the First Annual Review of the National Cancer Plan
- Signing Ceremony of the "PARAMED Project"
- Bangladesh Ambassador Informs Abiad of Donation of Essential Medicines for PHCs
- National Cancer Plan 2023-2028
- Abiad Represents Mikati at the Arab Medical Union Conference in Tripoli
- MoPH Affirms Its Previous Statement Regarding the Closure of Pastry Shop "Better from Scratch"
- MoPH Closes a Pastry Shop in Clemenceau for Causing Poisoning Cases
- Abiad Visites Nabih Berri Gov. Hospital and Inaugurates the Burns Treatment Department
- Developing “Minia Governmental Hospital” in a Meeting at the Ministry of Public Health
- Launching the National Mental Health Strategy in Lebanon 2024-2030 under the Patronage of the Minister of Health
- Abiad Inaugurates the Baabda Governmental University Hospital's Oxygen Generation Station
- A Detailed Presentation at MoPH on the Contingency Plan in the Event of Escalating Israeli Aggression
- Abiad Participates in the GHS2024 in Sydney and Met with Members of the Diaspora
- Abiad Concludes his Official Visit to Australia with a Series of Activities in Sydney
- Algorithm of Care
- Abiad Met with the Minister of Health in Melbourne and Held a Series of Meetings to Support the Health System
- MoPH Closes Two Beauty Centers and Two Clinics in Violation of the Laws
- MoPH Launches “Healing through Play” in Partnership with UNICEF, Denmark and the LEGO Foundation
- MoPH Launches in Collaboration with UNICEF the “RISING” Initiative to Promote Children’s Health
- Lebanon Elected in the Executive Council of Global Health in Geneva
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 738/1 & 739/1 Date 3/6/2024
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 595/1 Date 14/5/2024
- Stand at MoPH in Solidarity with the Medical Sector in the South
- Award for MoPH in Geneva in Recognition of Its Efforts on the “Step by Step” Programme
- MoPH Launches the National Campaign to Abstain from Smoking
- National Tobacco Control Campaign 2024
- MoPH and the Hospital Syndicate Organize a Protest in Solidarity with Health Workers and Hospitals in the South
- MoPH Condemns the Attack on Salah Ghandour Hospital
- School based surveillance
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 635/1 & 636/1 & 641/1 Date 15/5/2024
- A Field Inspection of the Arsal Camp for Displaced Syrians
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 540/1 Date 2/5/2024
- Antimicrobial Resistance
- Expanded Meeting at MoPH to Ensure that the Health Crisis in the Bekaa Does not Worsen
- Launching of the Arab Union for Optometry Professions Campaign “Vision for a Better Lebanon”
- Abiad Warns about the Outbreak of Diseases in Refugee Camps
- MoPH Receives a Donation of Cancer Drugs from the International Medical Corps
- UNHCR Inform Abiad of the Reduction in Health Coverage for the Syrian Refugees
- MoPH and MEHE Launch Anti-Smoking Awareness Campaign in Schools
- MoPH Announces 40 Cases of Viral Hepatitis A in Kamed al-Lawz
- National Intersectoral MHPSS Emergency Preparedness and Response Plan: In the Context of the Risk of War on Lebanon
- Abiad: The Dedicated Workers of Governmental Hospitals Deserve Praise and Support
- MoPH Warns of the Danger of Rabies
- Abiad Inaugurates the LSOG Annual Congress 2024
- MoPH Systems and Programs Shut Down Friday for Maintenance
- Abiad Visits Hazmieh PHC with French and EU ambassadors
- MoPH Refutes Several Inaccuracies in the Statement of the Order of Physicians in Beirut
- MoPH Demands the Sanctioning of the Attackers at Dar Al-Chifae Hospital
- MoPH Launches First-of-Its-Kind Tender to Bring together Guarantor Bodies to Procure Medicines
- Abiad Visites with the WHO Regional Director the Health Buildings in Karantina
- Abiad Organizes a Meeting with Controller Doctors as Health Coverage Increases Began to be Implemented
- Abiad Receives the Director of the WHO Regional Office for the Eastern Mediterranean
- Abiad Concludes his Meetings with Hospitals to Explain the Mechanism of the Large Increases in Coverage
- MoPh Denounces the Al Habbariyya Raid
- Abiad Explains to Hospital Directors in Beirut and Mount Lebanon the Coverage Increases
- Request for Quotation for Procurement of Goods Needed for the Turkish Hospital in Saida
- Abiad Explains the Big Increases in Health Coverage
- Abiad Inaugurates the Banin Association's PHCC
- Abiad Receives the Italian Ambassador in a Farewell Meeting
- Abiad Visits Bekaa to Explain the Mechanism of the Large Increases in Health Coverage
- Abiad Explains to Northern Hospitals the Mechanism of the Large Increases in Health Coverage
- Novel Coronavirus 2019
- New Solar Investment to Support the Health Sector in Partnership with UNICEF
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 280/1 Date 12/3/2024
- In Partnership with UNICEF Halabi and Abiad launch a School Health Screening Program with PHCs
- MoPH Clarifies Rumors about Rice Cooking, Shelf Life, and Toxic Substances
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 262/1 Date 6/3/2024
- MoPH Comments on Its Appeal to Hand Over the Body of a Child: It Happened Yesterday
- Abiad Discusses New Project with AFD
- Abiad Continues his Visit to Paris and Meets with the French Health Minister
- MoPH Regrets Delays in Drug Delivery Due to Public Administration Strike
- Excipients with Known Action
- MoPH Condemns the Israeli Occupation Forces' Insistence on Targeting Paramedics
- Abiad Embarks on an Official Visit to Paris to Discuss Projects to Modernize the Health Sector
- MoPH Organizes an Interactive Session on Cancer Awareness for 10th Graders at Lycee Abdel Kader
- MoPH, UNICEF and USAID Launch the Revitalization Universal Salt Iodization Program
- Abiad Inaugurates the Day Treatment Section for Cancer at the Turkish Hospital in Saida
- Health Drill at Siblin Governmental Hospital
- MoPH Condemns the Attack on the Islamic Health Society Center in Blida
- Look Alike Sound Alike Medicines
- Abiad Meets IOM Deputy Director General
- Abiad: We are Moving to a New Healthcare System, and Defining the Basic Package of Services is the First Step
- Abiad: The Battle Against Cancer is Great and Prevention is a Priority
- If You Have any Difficulty Calling the 1787 Hotline, Please Contact the Following Numbers: 01/615754-76/592699
- WHO Donates Six New Vehicles to MoPH’s Epidemiological Surveillance Unit
- Abiad Honors the Team of the National AIDS Control Program
- Laboratory based surveillance
- One Year Review for Lebanon National Health Strategy:Vision 2030
- Request for Quotation for Services for Call Center
- Abiad & Halabi Launch the National Cancer Awareness Campaign
- Revision of the National Guideline on Prevention and Management of Wasting in Lebanon
- Abiad in the First Evaluation Meeting of the National Health Strategy
- Abiad Launches “February, the Month for Oral Health in Children”
- Abiad Discusses with the New U.S. Ambassador the Status of the Health Sector in Lebanon
- Mental Health and Substance Use Strategy for Lebanon 2015-2020
- External mid-term evaluation of the Lebanon national Mental Health Strategy 2015-2020
- Abiad Visits the Karantina Warehouse and Public Hospital with a Delegation from the Republic of Korea and UNICEF
- Abiad Discusses Medical Sector Affairs with the Syndicate Council
- Medical center and dispensaries based reporting
- Abiad Renews the Call for an Immediate Ceasefire in Gaza
- Abiad from Nabatieh: The Medical Sector is Steadfast
- Abiad Met in Tyre with Directors of Governmental and Private Hospitals
- Abiad Inaugurates the Annual Scientific Conference on Psychiatry
- Monitoring of COVID-19 Infection In Lebanon - 10/1/2024
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 29/1 Date 9/1/2024
- How to Navigate the Cold and Flu Season?
- Abiad Reassures Patients of Cancerous and Chronic Diseases
- MoPH Denounces the Targeting of the Health Authority Center
- National Pharmacovigilance Program Newsletter-Issue 9- January 2024
- Drugs Public Price List 2023
- Successive Meetings about the Drugs at MoPH and Abiad Expects a Breakthrough in Funding
- Abiad Suspends the Contract with Bellevue Medical Hospital
- Mikati Discusses with Abiad Securing a Thousand Billion Lbp per Month for Cancer and Chronic Diseases Medicines
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 1795/1 & 1796/1 Date 20/12/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 1602/1 Date 28/11/2023
- MoPH Shares the Pain of Cancer Patients
- Abiad Inaugurated STMC Hospital at the Event: This is Evidence of the Health Sector’s Resilience
- Abiad Issues a Decree to Raise Kidney and Blood Dialysis Tariffs: We Stand by the Patient
- Abiad Visited Sheikh Al-Aql: The Citizen’s Interest is a Priority and Support Continues for Cancer Medicines
- Abiad During a Coordination Meeting with UNICEF: We are Moving Forward in Supporting PHCCs
- Abiad Visits Al-Shahar Al-Gharbi and Bchamoun Hospitals
- Abiad Calls at the WHO Meeting on Gaza for an Immediate Ceasefire
- Abiad Receives from the German Ambassador a Donation of Special Supplies for Treating War-Wounded People
- Capacity Building
- Abiad Closes the Al-Ayyas Butchery in Al Jahiliya and Refers the File to the Public Prosecution
- Abiad, the Japanese Ambassador, and the UNICEF Representative Inspect the Medical Supplies Warehouse in Karantina
- Investigation into the Causes of Dozens of Disease Cases in Jahiliya and Tests on Food and Water
- What’s the Impact of Climate Change on Health Systems?
- Explore Trusted Sources for Information on Health Emergencies
- MoPH Receives a Donation of Equipment and Supplies from the Czech Republic for Governmental Hospitals
- Abiad Receives a Donation of Medicines from Brazil
- Abiad Concludes its Meetings at COP28, and Calls for Regional Solutions to Local Health Crises to Prevent their Spread
- What are the PHCCs Programs and Services that you Can Benefit from?
- Abiad at the Meeting of Health Ministers at COP28
- Abiad Visits Hasbaya Governmental Hospital Accompanied by MPs Jarada and Hamdan
- Abiad at the Opening of the Neonatal Intensive Care Department at Baalbek Hospital
- Abiad Inspects Machghara Governmental Hospital: It is the Health Sector’s Duty to Remain Highly Prepared
- Abiad Opens the Ali Al-Nahri PHC: It is not Permissible for these Centers to Continue to Finance Themselves
- The Minister of Public Health Dr. Firass Abiad at COP28 in UAE
- MoPH Responds to Those Who Object to Tracking Nonsubsidized Medicine
- MoPH Alerts Citizens and Reminds them of Health Guidelines Related to White Phosphorus
- MoPH Follows on with the Training of Medical Personnel across all Lebanese Territories
- Ministry of Public Health Issues Health Guidelines on White Phosphorus
- MOPH Achievements to Enhance Transparency and Prevent Corruption
- Insights from the First Annual Pharmacovigilance Conference in Lebanon - 2023
- Abiad and the Spanish Ambassador Discuss the Ways to Support the Health Sector
- Abiad Chairs a Meeting of Directors of Governmental Hospitals in the North and Akkar
- Abiad: The Medical Sector is Highly Prepared to Confront any Attack or Aggression
- Abiad Checks on the Readiness of the Health Sector in Tripoli and the North
- Abiad Visited the Tripoli Fatwa House and Met with Mufti Imam
- Abiad Briefs Representatives of Donor Countries on the Health Emergency Plan: It Has Dual Effects in the Short and Long Term
- Abiad Participates in the Graduation of Nurses Who Participated in a Training Program at the IECD
- Acute Watery Diarrhea Surveillance in Lebanon
- Measles Surveillance in Lebanon
- MoPH Follows on with the Training of Medical Personnel across all Lebanese Territories
- World Diabetes Day 2023
- MoPH Distributes 50 Tons of Medical Supplies to 20 Governmental and Private Hospitals
- The Ministry of Public Health Strongly Condemns the Targeting of Mays al-Jabal Hospital
- MoPH Follows Carries on with the Training of Medical Personnel
- Abiad Launches Ibn Al-Nafis Medical Center: We are Working on Projects to Support these Centers
- MoPH Reumes Hospital Training to Increase their Prepardness
- Accreditation Certification ISQua EEA
- Abiad Inspects Tyre Hospitals, Shelters for Displaced Persons, and the Disaster Management Unit
- Abiad: The MoPH will Be alongside Hospitals in the South to Confront any Developments
- Abiad: Our Budget to Confront the Repercussions of any Aggression is $20 Million
- MoPH Condemns the Attack against Two Ambulances: A Flagrant Violation of International Humanitarian Law
- Abiad Meets with District Doctors and Agreement on a Communication Mechanism to Ensure Effective Coordination
- Abiad Sponsors the Medical Day for Promoting Mental Health and Preventing Addiction
- Collaboration between the MoPH, UNICEF and Korea to Support Life-Saving Care for Newborns
- Med Safety Week Starts Today
- Med Safety Week Starts Today
- Chemical Biological Radio Nuclear Events Preparedness (CBRN Program)
- The Regional Director of the WHO Meets with Abiad: The MoPH Turned Challenges into Opportunities
- The MoPH Activates a Hotline (1787) to Serve those Forcibly Displaced from their Areas
- Abiad Briefed the Syndicate of Private Hospitals on the New Mechanism for Covering the War-Wounded
- Abiad Issued a Memo to Hospitals on Preparedness for Emergencies
- Abiad Meets with the Deputy Executive Director of UNICEF and an Emphasize on Continued Support for the Health Sector
- Abiad Discusses with Wronecka the Health Emergency Plan
- Abiad Launches of the National Lead Poisoning Awareness Campaign
- Abiad Meets with the Ambassadors of Bangladesh and India and Discusses Supporting the Health Sector
- Abiad Discusses with the Ambassadors of Bulgaria and Pakistan ways of Cooperation to Support the Health Sector
- Abiad Discussed with UN Representatives Ways of Cooperation and Support for the Emergency Plan
- Call for volunteers in the health fields
- Abiad Tours with Alama and Abdallah in the PHEOC and Meets with the Colombian Ambassador
- Abiad Stops Contracting with Rahal Hospital after Causing Several Problems with Dialysis Patients
- Abiad: The Main Concern is Financing the Work of the Emergency Plan
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 1343/1 Date 17/10/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 1245/1 Date 3/10/2023
- Where Can you Find Affordable / Free Mental Health Services in Lebanon?
- The Qatari Ambassador Visits Minister Abiad and Discusses Qatari Support for Lebanon
- Results of the Laboratory Technician Proficiency Exams 2023-2024
- Mikati Participates in a Meeting at the MoPH to Discuss the Plan to Increase the Readiness of the Health Sector
- Abiad: To Stand for a Moment of Silence in Condemnation of what Happened at Baptist Hospital in Gaza
- Ministers Abiad and Hajjar Discuss Ways of Coordination to Follow up with Recent Events
- National Breast Cancer Awareness Campaign 2023
- Al Abiad: We are Working to Reactivate Awareness Campaigns and Comprehensive Coverage of Mammography
- Al Abiad Presents the Ministry’s Procedures to Increase Preparedness in the Event of any Emergency
- NHA Key Indicators 2019 - 2020 - 2021
- Al Abiad Raises in the Regional Session of the WHO the Need to Raise Health Preparedness in Anticipation of any Emergency
- National Health Accounts 2020
- Announcing a Study to Monitor NCD Risk Factors
- Al Abiad Launches the National Guideline of Good Pharmacovigilance Practices
- National Health Accounts 2021
- Al Abiad Opens the Fourth Conference on Neuro-Oncology at the American University
- Al Abiad during the Launch of the Seasonal Influenza Vaccination
- The Ministry of Public Health Lights its Building in Pink to Launch the Breast Cancer Awareness Campaign
- Al Abiad Visits Al Zarif Medical Center with the Danish Ambassador
- Health Indicators
- Barbara Nassar Association Launches Its First Center to Support Cancer Patients and Awards Minister Abiad
- Al Abiad: Physical Therapy is an Integral Part of the Primary Health Care Program
- Al Abiad Announces Securing Hospital Payments for Dialysis
- Al Abiad: The Holding of 6 Medical Conferences is Evidence of the Health System not Collapsing
- Al Abiad Discusses with the EU Deputy the Support for the Health System
- Request for Quotation:Procurement of Maintenance of Generators for the Ministry of Public Health
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1116/1 & 1117/1 & 1118/1 & 1131/1 Date 12/9/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 1141/1 Date 14/9/2023
- Al Abiad: Financing is the Greatest Challenge and International Solidarity with Lebanon is Necessary
- Al Abiad: The Syrian Displacement Exposes the Health System to Structural Weakness
- Abiad’s Meetings in New York to Enhance Cooperation with Partners in Health System Support Programs
- Al Abiad at the United Nations Meeting on Epidemics: Lebanon Deserves Special Attention
- Honoring of Al Abiad in Houston and Emphasizing the Medical Partnership Between Lebanese Residents and Expatriates
- Al Abiad Participates in the Lebanese American Medical Association Conference in Arizona
- A Series of Projects to Support the Health Sector in Abiad’s Meetings at the World Bank
- National Health Accounts 2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1090/1 & 1091/1 Date 6/9/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 1017/1 & 1022/1 Date 28/8/2023
- Al Abiad to the USA to Meet with World Bank Officials, Lebanese-American Medical Associations
- Al-Abiad Receives from Al-Saeedi 18 tons of Medical Aid Provided by the Sultanate of Oman
- Abiad: The Disbursement of Funds to Support Medicines for Cancer and Incurable Diseases will Take Place this Week
- Minister Abiad Represents Mikati at the Graduation of Jinan University Students
- Makari and Abiad Assist to a Dialogue Meeting Following Attieh's Invitation in Rahbeh
- The Minister of Health Visits Subul Al Salam Ambulance Service and was Briefed on Its Work
- Minister Abiad Sponsors the Opening of the Al-Iman Health Center in Bebnin
- Abiad Representing Mikati, Lays the Foundation Stone for the Dialysis Department at Al Minieh Gov. Hospital
- Minister Abiad Toured Four Governmental Hospitals in the North
- The Minister of Health Visited Ehden Gov. Hospital to Receive a Japanese Donation
- Service Coverage
- Minister Abiad Concluded his Visit to Paris with Meetings about the Cancer Plan and Digital Transformation
- Minister Abiad in France to Develop Quality Standards and Implementation of the National Cancer Plan
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 994/1 & 995/1 & 996/1 Date 22/8/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 977/1 & 980/1 Date 21/8/2023
- Minister Abiad Received a Donation from Islamic Relief for Four Governmental Hospitals
- Minister Abiad Released the Annual Reports of Maternal Deaths
- Clarification from the MoPH on News of the Spread of Hemophilia A in Baalbek-Hermel
- Minister Abiad is Discussing with the Australian Ambassador in Lebanon Projects to Support the Health Sector
- Clarification from the Ministry of Public Health
- Minister Abiad Chaired a Meeting of the Public Insurance Funds
- Abiad Met Mikati: The Situation of Coronavirus in Hospitals Is Under Control
- Case Study on the Digital Transformation of Health Systems in Lebanon
- The National E-Health Program
- Minister Abiad Visited LEMSIC Medical Students at Makhzoumi Healthcare Center
- Minister Abiad Discussed the Arrangements for Receiving Omani Medical Assistance
- Clinical Management of Rape (CMR) Facilities
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 922/1 Date 8/8/2023
- MoPH Closed a Restaurant in Kabrishmoun for Poisoning a Number of People
- MoPH Denies Inaccurate News about a New Wave of Corona
- Minister Abiad Chaired a Meeting Presenting the Procedures to be Applied in Nurseries
- Minister Abiad Received Representatives of the Health Sector from the Lebanese Private Sector Network
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 848/1 & 849/1 Date 27/7/2023
- The Minister of Health and the Secretary General of the Higher Relief Commission Inspected Saida Governmental Hospital
- Minister Abiad Inaugurated the New Building of Karantina Hospital
- Donation from Qatar Red Crescent to Equip Cancer Treatment Departments in the Governmental Hospitals
- Minister Abiad Toured Nabih Berri Governmental University Hospital in Nabatiyeh
- Minister Abiad Inaugurated the Solar Energy Project in Tibnin Governmental Hospital provided by Japan
- Minister Abiad Stressed that Food Safety Should not Be Compromised
- The Ministry of Public Health Announces the Evacuation of Patients from Saida Governmental Hospital
- Medicines Safety Takes Root in Lebanon
- Minister Abiad Launched an "Ambitious and Realistic" Vision for the Digital Transformation of the Health Sector
- Minister Abiad at the Opening of New Departments in Baabda Governmental Hospital, with an Italian Funding
- Vision for Digital Health Transformation
- A Delegation from the General Labor Union in Lebanon Visited the Minister of Public Health
- Minister Abiad Presided over a Meeting of the Cholera Control Committee
- Minister Abiad Discussed with the Lebanese Order of Pharmacists the Cooperation in the Drugs File
- Minister Abiad Announced the Withdrawal of the Child Abuse Nursery License
- The MoPH Participated in a Training Course at the National Institute of Administration "ENA"
- Minister Abiad Received Cancer Drugs from the Italian Ambassador
- Mikati at the Launch of the National Cancer Plan 2023-2028
- The Minister of Health at the Inauguration of "Norge" Baskinta Medical Center
- Minister Abiad, Participant in the "One Sustainable Health for All" Conference in Lyon
- Closing a Nursery for Child Abuse with the Red Wax
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 752/1 & 753/1 & 756/1 Date 4/7/2023
- 2017
- 2016
- 2022
- Service Delivery
- The MoPH Shuts Down Twelve Aesthetic Centers
- Acute Watery Diarrhea Surveillance in Lebanon- 19/6/2023
- Measles Surveillance in Lebanon- 19/6/2023
- Abiad and His Moroccan Counterpart Discussed Ways to Strengthen Bilateral Cooperation
- Minister Abiad Calls for Additional Support for the Health System
- Letter Related to the Nomination of Hospital Pharmacovigilance Focal Points.
- Abiad and His French Counterpart Signed a Framework Agreement for Coordination of Assistance Programs
- Request for Quotation: Provision of SMS Service
- Request for Quotation: Maintenance, Support and Update of the Ministry’s Application
- The MoPH Declares End of Cholera Outbreak in Lebanon
- Minister Abiad Met with a Delegation From North Lebanon
- The USJ Celebrates the Centenary of the School of Midwifery's Establishment
- Minister Abiad Stressed that Maintaining Quality Should Not Be Tolerated
- Minister Abiad Presents the Outcomes of Lebanon's Participation in the World Health Assembly in Geneva
- Cholera Surveillance in Lebanon- 2/6/2023
- The Order of Nurses in Lebanon Calls for Better Wages for the Nursing Sector
- Request for Quotation: Procurement of an Antivirus Software
- Request for Quotation: Procurement of Spare Parts for the Elevators at Al Nabatieh Public Hospital
- Request for Expression of Interest to hire an Environmental and Social Specialist and Grievance Mechanism Officer
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 563/1 & 564/1 & 569/1 & 570/1 & 571/1 & 572/1 & 573/1 Date 29/5/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 527/1 & 530/1 Date 18/5/2023
- Issuance of a New Drugs Public Price List No.23/2/15106 Date 5/6/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 476/1 Date 4/5/2023
- Abiad Participates in the Centenary Celebration of the USJ Faculty of Dental Medicine's Establishment
- Minister Abiad Opens the 2nd Levant Endocrinology and Diabetes Congress
- Abiad Took Part in the Awareness-Raising Campaign on the Harmful Effects of Tobacco Use
- Abiad and World Bank Delegation Examine Projects Aimed at Promoting Healthcare Services
- Abiad Participates in Beirut Lions Club's Ceremony Recognizing Top Nursing Students
- Abiad Discussed with the World Bank Delegation the Health Reality
- On the International Day of the Midwife, Abiad Stressed the Need for a Sustained Support for Midwives' Services
- WHO Regional Consultation Meeting on the Development of Vitamin D Guidelines in the Middle East
- Abiad Calls For Support to Primary Health Care During the Ophtalmologist Annual Meeting
- Abiad Introduced the Forthcoming National Cancer Plan in Geneva
- Minister Abiad Takes Part in WHO Meetings in Geneva
- Blood Transfusion
- Digital Health Retreat-2023
- The Second Session of the Digital Transformation Forum in the Health Sector
- Minister Abiad Congratulates Pr. Jamal Ayoubi on His Achievement
- Minister Abiad Launched Medleb Application that Enables the Patient to Check the Drug's Price
- The Minister of Health Dr. Firas Abiad Launches the Digital Health Retreat Forum
- Abiad Highlights the Positive Outcomes of the Digital Health Retreat Forum
- Awareness Meeting on the Media Coverage of Suicide
- Digital Health Retreat in the Health Sector
- The MoPH Shuts Down a Pharmacy and Refers 13 Supplies Import Companies to the Public Prosecution Office
- Abiad and Grillo Discussed Projects Funded by the Government of France for the Support of Gov. Hospitals
- UNICEF's Projects Promote the Role of Hospitals and Medical Centers, Abiad
- Abiad Kicks off his Tour of North Lebanon with a Visit to the Twins Rahaf and Riham
- The Second Training Session on Meditrack for the Pharmacies to Tracking Cancer Drugs
- Training Session on Meditrack Held at the MoPH for the Pharmacist Insepectors
- Minister Abiad Launched the Training Sessions on Meditrack for the Pharmacists
- Report on the Automated Mechanism to be Followed by the MoPH for Pharmaceutical Tracking
- Minister Abiad Chairs the Second Workshop on MediTrack System
- Steps to Obtain a Unique Health ID, Enter the Medical Record into Aman Program and Follow Up Through the Hotline 1214
- COVID-19 Symptom Checker and Virtual Consultation
- Abiad and the Ambassador of Japan Inaugurate the Solar Power Project at Minia Governmental Hospital
- COVID-19 Symptom Checker- Your Self-Help Guide for Coronavirus COVID-19
- New Procedures for Incoming Passengers starting 27/9/2022
- Issuance of New Decisions Related to Drug Pricing
- The Central Inspection's Audit Report on Ftouh Keserwan Hospital Submitted to Minister Abiad
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 297/1 Date 20/3/2023
- Conference on Cancer Prevention Held at the Beirut Bar Association
- Abiad and Hojairy Examine the Health Needs of Arsal's Residents
- Abiad Considers Ways to Ensure Continued Operation at Bar Elias Hospital
- Issuance of a New Drugs Public Price List No.23/2/11529 Date 3/5/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 347/1 & 349/1 & 352/1 Date 11/4/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 382/1 Date 18/4/2023
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 281/1&283/1&284/1&289/1 Date 14/3/2023
- Abiad Launches the Awareness Campaign on the Children Vaccination against Measles
- Awareness Campaign on the Children Vaccination against Measles- 2023
- Abiad and the Ambassador of the Czech Republic Brought up Health Support Projects
- Abiad and Zaiter Discussed the Project of Establishing a Governmental Hospital in Hrabta
- MediTrack to Include Additional Medicines for Incurable Diseases, Abiad
- Administrative Procedures for Patient's Access to Drugs through Meditrack
- Adverse Events Following Immunization Monitoring-Oral Cholera Vaccines-Lebanon-Phase I - II- III
- The MoPH Freezes Contract with the Rosary Sisters Hospital
- Issuance of Minister's Decision No. 412/1 of 25/4/2023 on Linking the Pharmacy Inventory Management System POS to MediTrack
- The National Strategy will Help Restructure the Healthcare System, Mikati
- Issuance of Memorandum No.8 on Measles Case Management in Lebanon
- The WHO Provides Lebanon with the First Batch of Insulin
- Medicines and Medical Supplies were Donated by the Council of Arab Ministers for Health
- Minister Abiad Visits Oasis de Vie Healthcare Center
- Minister Abiad Met with the President of the Order of Nurses in Lebanon
- Minister Abiad Reaches Agreement with Hospitals and Physicians to End the Dialysis Crisis
- Abiad and the Lebanese Association for Hemophilia Discussed Ways to Access Treatment Through Meditrack
- Joint Statement on the Media Coverage of Suicide
- Lebanon Health Resilience Project in Collaboration with the World Bank
- Minister Abiad Received Kidney Dialysis Patients
- Minister Abiad Receives a Donation of Medicines from Pakistan
- To All the Doctors Wishing to Attend a Training Course in Russia
- TB Program Strategic Plan Approach Announced
- Abiad and the Syndicate of Medical Supplies Importers Discussed Possible Solutions to Ensure the Patient's Right
- Minister Abiad Strongly Criticizes the Repeated Calls for Strike
- The Health Committee Discussed with Minister Abiad the Current Health Situation
- Issuance of Minister's Decision No. 276/1 of 14/3/2023 on the Amendment of Decision No. 228/1 of 6/3/2023
- World No Tobacco Day 2023
- World No Tobacco Day 2022
- The MoPH Opens an Investigation into the Incident at Sheikh Ragheb Harb University Hospital
- Issuance of Decision No.230/1 of 8/3/2023 on the Amendment of Decision No 945/1 of 3/10/2022 (Mechanism for Dispensing Drugs)
- Issuance of Decision No.231/1 of 8/3/2023 on the Formation of a Committee to Examine the Files of the Patients with Eye Diseases
- One Hundred Fifty PHCs Equipped with Solar Energy Systems with the Support of UNICEF
- Minister Abiad Met with the Importers of Heart and Kidney Dialysis Supplies
- The Order of Nurses in Lebanon Marks the Twentieth Anniversary of its Foundation
- S.A.I.D. NGO Launched Its Annual Campaign for the Early Detection of Colorectal Cancer
- Meeting at the Ministry on the Money Received by the Airline Companies from COVID-19 Tests
- Abiad Examines Ways to Coordinate Efforts to Implement the National Health Strategy's Priorities
- Minister Abiad Held Meetings with the World Health Organization in Lyon
- Minister Abiad Met with his French Counterpart in France
- Minister Abiad Held a Series of Meetings During his Visit to France
- Map of substance use and rehabilitation services in Lebanon
- Abiad Announces a Series of Cooperation Projects with the Organisation of European Cancer Institutes
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 143/1&147/1&148/1&149/1&150/1 Date 8/2/2023
- IBloodlink Mobile App
- Minister Abiad Visits Nabih Berri Governmental University Hospital in Nabatieh
- Abiad and the Newly Appointed UNHCR Representative Consider Ways to Enhance Health Sector Readiness
- Adverse Events Following Immunization Monitoring-Oral Cholera Vaccines-Lebanon-Phase I - II
- Minister Abiad Discussed with Donors and Partners Ways to Implement Health Strategy
- Request for Quotation: Procurement of Helium Tanks
- Request for Quotation: Procurement of IT Hardware
- Lebanon National Drugs Database
- The MoPH Confirms Nabih Berri Governmental Hospital Will Resume Normal Operation
- Update to the List of Products Exempted from the Implementation of the 2D Barcode
- Minister Abiad Chairs a Meeting to Coordinate the Health Sector Response to Disasters and Earthquakes
- Private Nurseries to Shut Tuesday and Wednesday Due to Seismic Events and Winter Storm
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 98/1 Date 25/1/2023
- Minister Abiad Introduced the National Health Strategy- Vision 2030
- Infection Prevention and Control (IPC)
- Minister Abiad Visits Al Makassed Hospital
- Issuance of a New Drugs Public Price List on 1/2/2023
- Launching of The National Health Strategy
- Opening of the Tuberculosis Center at Tripoli Governmental Hospital
- Lebanon National Health Strategy-Vision 2030
- Inauguration Ceremony of Solar Energy Project at Tripoli Hospital under the Patronage of Minister Abiad
- Minister Abiad Visits Al Makarem PHC and Orange Nassau Hospital
- Minister Abiad Briefed Mufti Imam on Health Projects For Tripoli Hospitals
- Issuance of a New Drugs Public Price List Modified on 27/1/2023
- Minister's Decision to Issue a Daily Index For the Prices of Unsubsidized Medicines
- Hospital Accreditation
- Issuance of a New Drugs Public Price List Modified on 25/1/2023
- Minister Abiad and Akkar MPs Brought up the Needs of the Region
- The MoPH Reports Huge Violations of Resolutions Regarding the Sale of Medical Supplies
- Press Conference on the First and Successful Surgery to Separate a Conjoined Twins at The AUB
- Abiad Says the Temporary Solution Ensures the Implementation of Pharmaceutical Tracking System
- Cooperation Agreement Signed Between Tripoli Governmental Hospital and Beirut Arab University
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 67/1 & 68/1 Date 17/1/2023
- Abiad Met with a Delegation of The Arab Hospitals Federation Headed by MP Allama
- Abiad and the Ambassador of Norway Discussed Epidemiological Surveillance Programs
- Minister Abiad Launched the New COVID-19 Vaccine Campaign at Saint George Hospital
- Minister Abiad Holds Meeting with Representatives of Governmental and Private Hospitals
- COVID-19 Pfizer Vaccination Centers
- National Pharmacovigilance Program Newsletter-Issue 5 (January 2023)
- National Awareness Campaign on COVID-19 Vaccine
- Cadic Reaffirms France's Continued Support for Lebanon's Health Sector
- Minister Abiad Meets the Ambassadors of Qatar and China
- The Decreasing State Income Impacted the Ministry's Services, Abiad
- The MoPH Announces Adjustment to Kidney Dialysis Session Tariff
- The National Immunization Campaign- 2022
- Awareness Campaign on Cholera 2022
- Inauguration of Surgery Departments at al-Zahraa Hospital Under the Patronage of Minister Abiad
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 1443/1 Date 28/12/2022 & 1450/1 Date 29/12/2022
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 28/1 & 29/1 Date 9/1/2023
- Abiad Met with the Ambassador of India, As He Expressed His Thanks to His Support to Health Sector
- Lifting Subsidies on Infant Formula Will Prevent Smuggling and Selling it on the Black Market, Abiad
- Drugs Public Price List 2022
- The MoPH Condemns the Attack on a Staff member At Miniyeh Hospital
- Minister Abiad Launches Renewable Energy Project at Sibline Governmental Hospital
- Abiad Says a new COVID-19 Wave Is Emerging in Lebanon But Is Still Under Control
- Abiad Met with Representatives of Health Insurers, as He Stressed on the Need to Abide by Cancer Medicine Tracking System
- The List of Approved COVID-19 PCR Testing Laboratories at the Governmental Hospitals
- Adverse Events Following Immunization Monitoring-Covid-19 Vaccines-Lebanon
- Introductory Video on the Med Safety App
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 1418/1 Date 20/12/2022
- The MoPH Receives 300,000 Doses of COVID-19 Vaccine Donated by France
- Oral Cholera Vaccination Campaign Program - Second Stage
- Minister Abiad Visits Rachid Karami Cultural Center
- Abiad Visits The Social Services Medical Center in Abi Samra
- Abiad Tours North Lebanon with Shea: The Cholera Outbreak Is Not Yet Over
- A Counterfeit Batch of Cancer Medicine METHOTREX 50 mg (Methotrexate) Recalled
- Revised Hospital Accreditation Standards in Lebanon- December 2022
- Revised Hospital Accreditation Standards in Lebanon- December 2022
- Adverse Events Following Immunization Monitoring-Oral Cholera Vaccines-Lebanon- Phase I
- We Have Been Able to Curb the Spread of Cholera, but the Outbreak Is not Yet Over, Abiad
- Minister Abiad Informs Drug Importers that Price Index Will be Issued on a Weekly Basis
- List of Authorized IRBs
- The UN Humanitarian Coordinator Affirms Commitment to Support Lebanon's Health Sector
- Abiad and the Syndicate of Medical Supplies Importers Discussed Ways to Avoid Shortages
- Minister Abiad Receives Donation of Medicines From Qatar
- Lauching of the Lebanese National Strategic Plan to End TB for 2023-2030
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 1261/1 & 1280/1 & 1283/1 & 1290/1 Date 6/12/2022
- Minister Abiad Launches The Second Stage of Cholera Vaccination Campaign
- The MoPH Deplores the Repeated Attacks on Medical and Nursing Staff
- List of Bottled Water Permitted by MOPH
- Charges for IV Cancer Drugs Administered in Hospitals Will Be Listed on Hospital Bill, Abiad
- Minister Abiad Received a Donation of Prosthetics from India
- The Collaborative Governance of Lebanon’s Health Sector
- Sassine and Cheaito Briefed Abiad on the Outcome of The Arab League Strategy to Promote Nursing and Midwifery
- We are Working Hard to Ensure Access of Dialysis Patients to Treatment at No Additional Cost, Abiad
- Gavi Representatives Commend the MoPH for Its Effective Vaccination Plan
- Abiad Confirms Cholera Outbreak Under Control
- The MoPH Recalls the Conditions for the Import of Food Supplements to Lebanon
- Minister Abiad and The British Ambassador Discussed the Country's Health Challenges
- Abiad Inaugurates Neonatal Care Unit at Baalbek Governmental Hospital
- Launching of Sustainable Energy Strategy in Healthcare Sector
- Minister Abiad Met with UNICEF Regional Director
- Minister Abiad Met with UN High Commissioner for Refugees Filippo Grandi
- Launching of the Cholera Vaccination Campaign in Nursing Homes
- The MoPH Launches Emergency Health Intervention at Elderly Nursing Home in Abou Samra
- Abiad Visits Baalbek Health Center at the End of his Tour of Baalbek
- Support is Needed for Healthcare Workers and the Communities Hosting Displaced Persons, Abiad
- Minister Abiad Visits The Islamic Hospital, Tripoli
- Abiad Visits Batroun Hospital: The Gov. Hospitals are Devoting Serious Efforts, but Need Support
- Abiad Opened the Lebanese German Forum 2022 – Health Innovations and Artificial Intelligence
- Haykal Hospital Holds Its 5th Annual Congress: COVID-19 In Rearview Mirror Amidst the Economic Crisis
- Minister Abiad Visits the Chamber of Commerce Tripoli
- Abiad and a Delegation of Institut Mérieux Discussed Ways to Develop a National Strategy for Laboratories
- Abiad Opened the Second Conference of the Arab Society for Nuclear Medicine
- Minister Abiad Launched the National Campaign for Newborn and Preterm Infants
- Hasan Launched with The WHO MediTrack System For Pharmaceuticals Traceability
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 1130/1 Date 14/11/2022
- The AUB Launched the Lebanese National Guidelines on the Uses of Vitamin D
- 190,000 Doses of Cholera Vaccine Have Been Administered to Date, Abiad
- The Lebanese Society of Obstetrics & Gynecology Presented to Abiad"Pregnancy during Cholera Outbreak"Protocol
- No Tobacco Control Program
- Minister Abiad Announces the Introduction of the Rotavirus Vaccine into the National Vaccination Programme
- Oral Cholera Vaccination Campaign Program - First Stage
- Red Cross Cholera Support Hotlines: 1760 for Case Follow-up and 140 for Patient Transport to Hospitals
- List of psychologists with a license to practice in Lebanon
- Abiad and al-Rami Stressed on the Need to Abide by the Precautionary Measures to Prevent the Spread of Cholera
- Abiad Closes the National Mental Health Campaign
- Abiad Attended the Congress of the Lebanese Society For Endocrinology, Diabetes and Lipids
- The Cholera Vaccination Campaign Targeted 34,237 People on Its Second Day
- Minister Abiad Annouces Pierre Fabre Donation of Cancer Medicines
- Abiad Oversees the Vaccination Campaign in the Village of Hisah, Akkar
- Abiad Received 600,000 Doses of Cholera Vaccine
- Minister Abiad Visits Bint Jbeil and Tebnin Governmental Hospitals
- Abiad Opens a Conference in Nabatieh-Cholera Outbreak 2022- Updates - Response-
- The Cholera Vaccination Campaign will Start next Saturday, Targeting People in the North and Beqaa, Abiad
- Abiad To Receive a Donation of Cholera Vaccines and Medicines from Egypt
- The MoPH Shuts Down a Nursery in Bchamoun after a Toddler Harmed an Infant
- Minister Abiad Announces the First Stage of the National Plan for Cholera Vaccination Campaign
- Drugs Public Price List 2021
- Abiad Tours Baalbek Hermel in Preparation for Cholera Vaccination Campaign
- The Immunisation Campaign to Begin Next Saturday First in Akkar and Bebnine, Abiad
- Minister Abiad Concludes his Tour of North Lebanon
- Abiad Tours Mahmra and Wadi Jamus, as He Announces Cholera Vaccination Campaign To be Launched Next Saturday
- Abiad Visits Salamtak PHC Center in Tal Hayat
- The Security Forces: The Vaccination Campaign against Cholera in Prisons Kicks off
- Abiad Visits the Lebanese People's Aid Center in Akkar as He Follows Up the Cholera Vaccination Campaign
- Minister Abiad Launched the Vaccination Campaign against Cholera from Halba Governmental Hospital
- Abiad Received In-Kind Donation from the Syndicate of Pharmaceutical Industries
- Abiad and a Delegation of the World Bank Visited Karagheusian Primary Healthcare Center
- Minister Abiad and The Danish Ambassador Discuss Health Cooperation Projects
- Lebanon Receives 13440 Doses of Cholera Vaccine Donated By France
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 1001/1 Date 12/10/2022
- Minister Abiad Inaugurates the Solar Energy Project at Rachaya Hospital
- Abiad Opens the Tenth Congress of The Lebanese Society for Quality and Safety in Healthcare
- Minister Abiad Met with a Delegation of the WHO to Discuss the Latest Updates on Cholera Outbreak
- Ministers Abiad Awards Medals of Honour to Four Women for COVID-19 Combat Work
- Ministers of Health and Industry Brought up Ways to Curb the Spread of Cholera
- Workshop on the Safe Transport of Patients with Cholera to Hospital
- Abiad Participates in the Signing Ceremony of a Protocol in Support of the PHCs
- Minister Abiad Looks into the Preparations for the Opening of a Field Hospital in Dannieh
- The MoPH Acting Director General Receives the Officer Medal of the National Order of Cedar
- The MoPH Director of Medical Care Awarded the Silver Medal of the National Order of Merit
- National Awareness Campaign on COVID-19 Vaccine during Easter Holidays 2022
- joseph
- Lebanon to Receive 600,000 Doses of Cholera Vaccine within the Next Two Weeks, Abiad
- Minister Abiad and the Italian Ambassador Oversee the Rehabilitation Works at Baabda Hospital
- A Field Hospital for Patients with Cholera Starts to Operate
- The MoPH Issues a Decision on the Full Coverage for Suspected and Confirmed Cases of Cholera
- Abiad: The First Part of Cholera Vaccine will be Provided to the Hospital Staff
- Abiad Inspects the Epidemiological Situation and Outbreak Response Measures in Arsal
- Minister Abiad Reaches Bebnine, as He Stresses on the Need to Provide Clean Water
- Minister Abiad Visits Tripoli Governmental Hospital
- Abiad Visits Microbiology, Health and Environment Laboratory (LMSE), Tripoli
- Minister Abiad Launched the Hospital Evaluation and Accreditation System in Lebanon
- Abiad Tours Tripoli: We Are Taking the Necessary Measures to Prevent the Spread of Cholera
- Memorandum No.41 Issued on 20/10/2022 on Cholera Case Management in Lebanon
- MoPH's Decision on the Mechanism for Dispensing Unsubsidized Medicines
- Minister Abiad Announces the Rapid Spread of Cholera
- Virtual Participation of Minister Abiad in the Meeting of the WHO regional Committee
- The MoPH Receives a New Batch of Assistance from Qatar Fund For Development
- Minister Abiad Announces The Unified Platform In Response to The Outbreak of Cholera
- Abiad and a Delegation of The European Union Discuss Ways to Enhance Cooperation Projects
- Minister Abiad Takes Part In The Annual Meeting of The Lebanese Society of Rheumatology
- The Ministry Will Provide the Coverage For the Lebanese Cholera Patients
- Abiad and a Delegation of International Organizations Visit Arsal Camps and Hermel Governmental Hospital
- Monkeypox Surveillance in Lebanon
- Hepatitis A Surveillance in Lebanon
- Minister Abiad and Representatives of Serum Industries Look into Ways to Respond to Cholera
- Mikati Chaired the First Meeting of the Committee on Cholera Control; Measures are Taken to Curb Its Spread
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 959/1 & 960/1 Date 4/10/2022
- The Lack of Clean and Safe Water Will Lead to the Rapid Spread of Cholera, Abiad
- We Have Seen a Sharp Decline in the Level of Basic Services in Akkar, Abiad
- Minister Abiad Visits el- Dinnieh: We are Working to Prevent the Spread of Cholera
- Abiad Started his Tour in Akkar with a Visit to a Refugee Camp and Dr Abdullah Al-Rassi Governmental Hospital
- Minister Abiad Met with European Ambassadors, Urging them to Continue Backing Lebanon During this Situation
- test
- test
- test
- test
- test
- test
- Awareness Campaign on Cholera 2022
- test
- Awareness Campaign on Cholera 2022
- test
- test
- test
- Awareness Campaign on Cholera 2022
- test
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Awareness Campaign on Cholera 2022
- Abiad Introduced Measures to Ensure High Level of Preparedness for Cholera Prevention
- The Ministry of Public Health Reports First Case of Cholera in Akkar
- Minister Abiad Takes Part in The World Innovation Summit for Health, Doha
- Minister Abiad Announces the Increase in Healthcare Coverage and Decisions to the Benefit of the Patient
- Japan and the UNOPS Support RHUH With Solar PV Systems and Medical Supplies
- japan
- japan
- Minister Abiad Chairs the First Meeting of the Working Group Tasked with Drawing up a Plan for PHC Promotion
- Minister Abiad and the Qatari Delegation Discussed Qatar's Initiatives to Support Lebanon's Healthcare Sector
- The Nephrologists Call on the Insurers to Secure Their Rights
- Meeting Between Minister Abiad and the World Bank Delegation on the Collaboration to Promote PHC Services
- Minister Abiad Chairs the First Meeting of the National Committee For Hospital Assessment and Accreditation
- Issuance of Decision No. 904/1 on the Exemption From COVID-19 Testing For Passengers at All Crossing Points
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 890/1 & 907/1& 912/1 Date 27/9/2022 & 28/9/2022
- Issuance of a Memorandum No.31 Regarding the Updated Recommendations for COVID-19 Isolation and Quarantine Period
- "Vee Laser Clinic" and Its Branches Shut Down By Minister's Decision
- Strengthening Lebanon's COVID-19 Response Project in Collaboration with the World Bank
- Minister Abiad Launched the National Pharmacovigilance Programme
- Abiad and His Syrian Counterpart Followed Up Transfer of Bodies and Injured People of Migrant Boat
- Joint Coordination with the Pediatric Society under the National Immunization Program
- Administrative Services
- Launching of the National Pharmacovigilance System
- The MoPH Conducts a Survey Entitled " Parent's acceptance of Pediatric COVID Vaccine"
- Abiad and Bombardieri Discussed Projects Funded by the Italian Embassy
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 812/1 Date 6/9/2022
- The Minister of Public Health Met with the President of Beirut Arab University
- Minister Abiad Chairs the First Meeting of the Joint Committee for Medicine Tendering
- Minister Abiad Met with the Senior Adviser of The World Diabetes Foundation
- A Delegation of the MoPH Visits the Islamic Charitable Hospital in Tripoli, Expressing Solidarity with its Staff
- The MoPH Condemns the Attack on a Physician at Tripoli's Islamic Hospital
- 34 Governmental Hospitals and 14 Health Facilities Received Diesel Donation from Qatar Fund For Development
- Minister's Circular Urging all Hospitals Not to Allow Patients to Leave the Emergency Unless After Providing a Bed for Them
- National Pharmacovigilance System Launching in Lebanon
- Minister Abiad Shares the Preliminary Findings of the Investigation
- Minister Abiad Inaugurates the Oral Health Section at Karagheusian Primary Healthcare Center
- Minister Abiad Discussed with MP Abdallah Projects Related to Healthcare Sector
- The MoPH Conducts an Investigation into the Death of a Patient in one of Beirut's Hospitals
- The MoPH: Training Sessions on Beauty Care Cancelled for Being Conducted by Frauds
- Minister Abiad Discussed with the World Bank Delegation Collaboration Projects
- Minister Abiad Met with the Newly-Appointed Ambassador of Iran
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No. 755/1 & 756/1 & 757/1 & 758/1 Date 18/8/2022
- The MoPH Shuts Down an Aesthetic Center in Down Town For Operating without a Legal License
- The MoPH: None of the Ministry's Employees is Involved in the Reported Theft of Money Allocated for Physicians
- The MoPH: Preventive Measures to Be Followed Inside Beirut Port and in Its Surroundings after the Air Test Results were Released
- Reminder of the Preventive Measures Related to the Potential Collapse of New Parts of Beirut Port Silos
- Abiad Held Two Meetings with Oncologists and Cancer Societies
- Minister Abiad Announces Investigation into Reported Shortage of Cancer Medicines
- The MoPH Reveals the Amount of Baby and Infant Formula Made available on the Market
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 524/1 Date 23/5/2022
- The MoPH Receives Third Financial Assistance from Qatar Fund For Development
- Minister Abiad: The BDL Pays on a Regular Basis the Amounts Due For the Dialysis Supplies Companies
- Minister Abiad Confirms in a Meeting that Baby and Infant Formula will be Made available on the Market
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 700/1 Date 2/8/2022
- Minister Abiad Toured Chouf's Health Centers and Visited Jezzine Governmental Hospital
- Launching of the USJ - HDF Hospital Network
- Minister Abiad Received Donations of Medicines and Medical Supplies from Turkey
- Abiad Signed a Memorandum of Understanding for Cooperation with Medical and Pharmacy Student Volunteers
- Minister Abiad Met with the World Bank Delegation to Examine Projects in Support of Primary Health Care
- Preventive Measures Announced with Regard to the Potential Collapse of Parts of Beirut Port Silos
- Awareness Campaign on COVID-19 2022
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 612/1 Date 20/6/2022
- Qatar Fund for Development Supports the Lebanese Health Sector with Monthly Aid
- Minister Abiad Received Donations of Medicines about $400,000
- Qatar Fund for Development Funds Health Sector in the Republic of Lebanon
- Coming Soon:
- Minister Abiad Met with Najat Rochdi and Thanked her for her Efforts to Support the Health Sector
- Adverse Events Following Immunization Monitoring-Covid-19 Vaccines-Lebanon-14th February 2021-June 30th 2022
- Services & Forms
- Partnership Agreement to Support Tripoli Governmental Hospital's Medical Services
- Minister Abiad Chairs a Meeting to Discuss the Situation of the Dialysis Patients
- Abiad Visits Hasbaya Hospital: Let's Work together in the Interest of the Citizen
- Abiad: Some of the Cancer Medicines are Now Available
- Minister Abiad Visits Marjaayoun Governmental Hospital
- Minister Abiad Toured the Primary Health Care Centers In Western Beqaa
- Abiad Chairs the Meeting of the COVID-19 Committee
- Minister Abiad Calls for Increased COVID-19 Vaccine Uptake to Curb the Spread of the New Wave
- The MoPH Instructs all the Hospitals in Northern Lebanon to Admit The Injured at Its Own Expense
- Nutrition
- الأبيض ترأس اجتماعا بحث في اوضاع مرضى غسيل الكلى
- Pfizer Marathon Week from 4 to 7 July 2022
- Public Health Advice for Gatherings during the current Monkeypox Outbreak
- Postponement of Colloquium Test for Licensed Medical Laboratory Technologists
- Minister Abiad Presents the Outcomes of his Visit to Washington
- The MoPH: A Clinic Run by Two Persons Posed as Plastic Surgeons Closed in Bourj Hammoud
- The Beqaa Health Service Closed 4 Butcher Shops for Selling Contaminated Meat
- Issuance of Minister's Decision No.619 on Putting the Drugs that haven't been Imported within a Period of Three Months
- The MoPH Recommends Adherence to COVID-19 Preventive Measures, Stressing the Importance of Vaccination
- ststistics 2020-test
- Statistics 2020
- Issuance of a new Drugs Public Price List Modified on 20/6/2022
- The MoPH Pursues Open Investigation into the Death of the Child Yasmine
- The MoPH Confirms First Case of Monkeypox in Lebanon
- The Reported Possible Cases of Monkeypox are Being Investigated and Samples are Sent for Testing
- The MoPH Confirms 174 Cases of Jaundice and Calls on to Obtain the Information Exclusively from the Ministry
- Minister Abiad Heading to Washington to Participate in the World Bank Health Financing Forum
- Abiad and Bakhash Discussed Ways to Ensure Better Coordination in the Patient's Best Interest
- The MoPH: This is the Reason behind the Spread of Hepatitis A
- Minister Biography
- Handover of the Karantina Supplies Warehouse after Reconstruction and Rehabilitation
- الصحة تسلمت مستودع الكرنتينا للمعدات واللوازم الطبية بعد إعادة تشييده وتأهيله
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 446/1 Date 9/5/2022
- The MoPH Proceeded with the Testing of Drinking Water in Tripoli after 49 Cases of Hepatitis A Had Been Reported
- The Media Office of Minister Abiad Announced He Had Tested Positive for COVID-19
- List of the Dietitians Registered with the Ministry of Public Health up To May 2022
- The MoPH Referred the File of the Governmental Hospital Incident to the Central Inspection
- The MoPH Announced an Investigation Into the Incident that Occurred in one of the Governmental Hospitals
- List of Candidates for the Position of President and Member of the Council of the Syndicate of Dietitians
- Coordination Meeting at the MoPH to Launch a National Strategy on the "World No Tobacco Day"
- The Minister of Public Health Announced that an Agreement Had Been Reached on the Funding for the Central Laboratory
- The Student Delegation that Took Part in the World Health Assembly Stressed the Need to Provide Medical Support to Lebanon
- Taamim No. 23 on the Identification of Monkeypox cases
- The MoPH Understands the Reasons which Led the Physicians and Hospitals Staff to Protest, but not at the Expense of Patients
- Minister Abiad Addressing the WHO General Assembly: The International Community must Support Lebanon
- Abou Charaf: There Are no Confirmed Cases of Monkeypox in Lebanon So Far
- Minister Abiad: The Health System Needs Solidarity of all Stakeholders
- The MoPH: There Is no Confirmed or Suspected Case of Monkeypox in Lebanon
- Antibiotic Awareness Campaign 2022
- The MoPH's Announcement for the Election of the President and Council of the Syndicate of Dietitians
- National OTC Medicines List
- Minister Abiad Met with Representatives of Cancer Patient Societies
- Form to be Filled by Psychiatrists in the Primary Health Care Centers when Prescribing for Specialized Psychotropic Medication
- Minister Abiad's Office Reaffirms that there is no Intention to Lift Subsidies for Cancer Medicines
- All Nurseries in Lebanon Will be Closed Next Monday
- Abiad: Our Efforts are Made First and Foremost Towards the Patient's Needs
- Abiad: The Medicines are Stored in the Refrigerators and we Urge all Concerned to Find Sustainable Solution for Drug Supply Center
- Baby Friendly Hospital Initiative
- International Health Regulations
- The Order of Pharmacists in Lebanon Launched a Sustainable Strategy for Medicines
- Minister Abiad Met with a Delegation of the UN Committee against Torture
- The Ministry's Director of Medical Care: The New Dialysis Tariff Provides Some Support to Patients
- Abiad during the Centenary Celebration of Hotel Dieu Hospital: The Lebanese Will Overcome Obstacles
- Minister Abiad Chairs a Meeting of the Supreme Health Council to Strengthen Resilience of Health Sector
- Adverse Events Following Immunization Monitoring-Covid-19 Vaccines-Lebanon- 14th February 2021- April 15th 2022
- Minister Abiad: Funding the Import of Medicines on the Agenda of the Upcoming Cabinet Session
- Minister Abiad Launched the National Immunization Campaign
- Health Minister's Office: The Demands of the RHUH Staff are not Treated with Disregard
- The MoPH Instructs Northern Hospitals to Admit the People Injured after Migrant Boat Capsized
- National Campaign on Measles and Polio Immunization 2020
- A Butcher Shop Shut Down over Selling Mixed Meat as Fresh
- Minister Abiad Inspects the Psychiatric Hospital of the Cross
- Minister Abiad Issues a Decision to Increase the Tariff of Dialysis Sessions
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.364/1 Date 4/4/2022
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.355/1 Date 31/3/2022
- Minister Abiad Received a Donation of Solar Power Systems from Japan at Baabda Governmental Hospital
- The MoPH Warns against the Consumption of the Poisonous Puffer Fish
- Health Expenditure
- The MoPH Requests Recall of Kinder Products over Potential Salmonella Contamination
- Abiad Communicated to The Importers the Council of Ministers' Approval to Transfer Money for the Import of Medicines
- The MoPH Confirms that Morphine-like Drug Is available in the Market
- National Awareness Campaign on Routine Immunization 2022
- The Ministry of Public Health Warns People against the Danger of Eating Mushrooms
- National Awareness Campaign on COVID 19 during Ramadan 2022
- The Ministry of Public Health Explained the Reason Behind the Shortage of Morphine
- Results of Students Applying for Competency Exams for Laboratory Technician License 2022
- Abiad: Patients shouldn't Be Turned Down and I will Help Hariri Hospital's Employees while Abiding by the Law
- The World Health Organization Launched the National Health and Environment Strategy in Lebanon
- Minister Abiad: COVID-19 Committee to Ease the Measures Related to the Pandemic
- Tobacco Awareness Campaign during the Month of Ramadan 2022
- The Implementation of Corrective Measures for the Pharmaceutical Policy Aims at Supporting the Patient's Medicines
- Minister Abiad Met with a Group of Protesters: I am Keen to Find the Possible Solutions
- TB Awareness Campaign 2022
- Minister Abiad Held Meetings in Qatar to Increase Collaboration Projects and Provide Support for Hospitalization
- Tuberculosis Screening Campaign in all the Tuberculosis centers
- Minister Abiad Addressed the Council of Arab Ministers of Health in Cairo
- Minister Abiad Launched the Guidance on Child Protection to Health Care Providers
- Mikati, Abiad and Boujikian Launched the Second Stage of Rationalizing the Support of Local Pharmaceutical Insdustry
- List of Moderna Vaccination Centers
- List of Pfizer Vaccination Centers
- Ministers Abiad and Boujikian Visited Benta Industries in Dbayeh and Algorithm Company in Zekrit
- Ministers of Public Health and Industry Visited Arwan Pharmaceutical Industries in Jadra
- Minister Abiad Participated in the Meeting on Health and Migration Held in Istanbul
- Minister Abiad Met with the Boards of Directors and the Coordination Body of the Governmental Hospitals
- Abiad Toured Hospitals and Medical Centers in South Lebanon: Our Aim is to Strengthen Primary Health Care
- Minister Abiad Met with his Egyptian Counterpart and the WHO Regional Director in Cairo
- Abiad Takes Part in The Arab Hospitals Federation Forum
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.272/1 & 273/1 & 274/1 Date 15/3/2022
- Minister Abiad Visits Sir Denniyeh Gov. Hospital: We Will Work as Best we Can to Support It
- Abiad: the MoPH is in the Process of Opening Kidney Dialysis Centers
- The Minister of Public Health Visits the Municipality of Tripoli: the North is a Deprived Area
- Abiad Received Medicines for Cancer and Chronic Diseases from Tunisia
- Minister Abiad Inaugurates the Drug Warehouse after Reconstruction
- Minister Abiad Brought up the Issues Facing the Import of Medicines
- PCR Results of Flights That Arrived on 25&26&27-2-2022
- Minister Abiad: I Received Assurances of Sustained Support to Lebanon
- The MoPH Ensures that Safe and Effective Vaccines are Strictly Used
- Minister Abiad Inaugurates a Neonatal Intensive Care Unit at Rafik Hariri University Hospital
- Elections of the Council of the Syndicate of Psychotherapists and Psychoanalysts to be Held Tomorrow
- Adverse Events Following Immunization Monitoring-Covid-19 Vaccines-Lebanon
- Adverse Events Following Immunization Monitoring-Covid-19 Vaccines-Lebanon
- Accepted Applications Nominated for Positions of Head and Member of Syndiacte of Psychologists
- The MoPH Announces the Closure of the UAE Center Following the Drop in the Number of COVID-19 Cases
- MoPH to Start Tomorrow a New Phase of Vaccination Campaign with the Administration of Pfizer and Moderna Vaccines
- Minister of Public Health Speaking at High-Level Debate on "Galvanizing Momentum for Universal Vaccination" at the UN
- PCR Results of Flights That Arrived on 19&20&21&22&23&24-2-2022
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.193/1 Date 22/2/2022
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.163/1 Date 15/2/2022
- Launching of the Field Epidemiology Training Program
- All Incoming Passengers who are Vaccinated within the Last Six Months will Be Exempt From PCR Tests
- PCR Results of Flights That Arrived on 17&18-2-2022
- PCR Results of Flights That Arrived on 11&12&13&14&15&16-2-2022
- PCR Results of Flights That Arrived on 11&12&13&14&15&16-2-2022
- Training for Vaccine Centers on Moderna 2
- Training for Vaccine Centers on Moderna 1
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.82/1 Date 26/1/2022
- COVID-19 National Vaccination Campaign FAQs about COVID-19 Vaccine
- MoPH Publishes List of Drugs that have Arrived and that will Arrive to Lebanon
- Request for Quotation for the Procurement of Vaccine Accessories
- PCR Results of Flights That Arrived on 5&6&7&8&9&10-2-2022
- PCR Results of Flights That Arrived on 5&6&7&8&9&10-2-2022
- Minister of Health Confirms that the Breach on MOPH PASS Platform was Handled
- Maintenance on MOPH PASS Platform
- Minister of Health Requests to Tighten Security Measures and to Investigate the MOPHPASS Platform Breach
- COVID-19 National Vaccination Campaign FAQs about COVID-19 Vaccine
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.56/1 Date 19/1/2022
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.29/1 Date 17/1/2022
- The World Cancer Day Meeting under the Patronage of Prime Minister Mikati at the Grand Serail
- PCR Results of Flights That Arrived on 29&30&31-1-2022 & 1&2&3&4-2-2022
- Minister Abiad and the Medical Sector Syndicates Agreed that the Security of the Hospitals Should Be Strengthened
- MoPH Statement on How to Obtain the PCR Result through the MOPH PASS
- Minister Abiad Chairs the Meeting of COVID-19 Committee: There is no Need for a Lockdown
- Abiad Assigns the Head of Medical Care Directorate to Investigate Into the Death of the Child Siham Chahine
- Minister Abiad Visits Al Makassed Hospital: It Is Our Duty to Support the Hospitals that Serve the Citizens
- The MoPH's Procedure to Gather the Vaccine Doses Administered Inside and Outside Lebanon in the Lebanese Certificate Exclusively
- PCR Results of Flights That Arrived on 26&27&28-1-2022
- PCR Results of Flights That Arrived on 22&23&24&25-1-2022
- Abiad: The File of the Airport's PCR Test Money Now Before the Court of Audit
- Minister Abiad Announces a Paradigm Shift in Medicine Tracking
- PCR Results of Flights That Arrived on 18&19&20&21-1-2022
- MOPH PASS Down for Maintenance Today, January 21, 2022 from 5 to 6 pm, Beirut Time
- The MoPH Confirms that the Vaccines Can still be Used for Three More Months
- PCR Results of Flights That Arrived on 15&16&17-1-2022
- Resolution No. 68/1 of 19/1/2022 on Cooperation Between the Ministry of Public Health and the Order of Pharmacist of Lebanon
- PCR Results of Flights That Arrived on 13&14-1-2022
- PCR Results of Flights That Arrived on 13&14-1-2022
- PCR Results of Flights That Arrived on 10&11&12-1-2022
- PCR Results of Flights That Arrived on 10&11&12-1-2022
- PCR Results of Flights That Arrived on 7&8&9-1-2022
- PCR Results of Flights That Arrived on 7&8&9-1-2022
- TB Awarness Campaign 2021
- Mikati Inaugurates Bin Zayed Center for COVID-19 Patients
- Minister Abiad Concludes his Tour with a Visit to Kana Governmental Hospital
- The Vaccine Executive Committee: COVID-19 Vaccine Registration Now Open to Children 5 through 11 Years Old
- Minister Abiad Receives from the Ambassador of Denmark 429,000 Doses of Moderna Vaccine
- الأبيض تسلم من سفيرة الدنمارك كمية من لقاحات موديرنا: لرفع المناعة المجتمعية والبدء بتسجيل الفئة العمرية بين 5 و12 سنة
- الأبيض تسلم من سفيرة الدنمارك كمية من لقاحات موديرنا: لرفع المناعة المجتمعية والبدء بتسجيل الفئة العمرية بين 5 و12 سنة
- Memorandum No.1 of 12/1/2022 Issued by the Minister on the Updated Period of COVID-19 Isolation and Quarantine
- Memorandum No.1 of 12/1/2022 Issued by the Minister on the Updated Period of COVID-19 Isolation and Quarantine
- Inauguration of Sheikh Mohamed Bin Zayed Center For COVID-19 Patients Tomorrow at Beirut Waterfront
- Abiad: There Is a Breakthrough in the Medicine Issue, the Infant Formulas to Be available as of Tomorrow
- Abiad during his Visit to Mays El Jabal Hospital: We are Working to Support the Governmental Hospitals
- Minister Abiad Visits Tibnin Governmental Hospital
- Minister Abiad: The Hospital Occupancy Rate is Equal to One Third of Last Year's
- Abiad Visits Siblin Hospital: The Vaccine will Save us from the next Tsunami
- Minister Abiad Inspects the Vaccination Center at Sidon Hospital
- The MoPH Reduces the PCR Cost at the Airport
- PCR Results of Flights That Arrived on 4&5&6-1-2022
- PCR Results of Flights That Arrived on 3-1-2022
- National Pharmacovigilance Program Newsletter-Issue 1 January 2022
- PCR Results of Flights That Arrived on 3-1-2022
- وزير الصحة من مستشفى ميس الجبل: نسعى لدعم المستشفيات الحكومية
- Pfizer Marathon to Take Place this Weekend, Targeting the Educational Sector and anyone who Wants to Take the Vaccine
- Procedures for All Incoming Passengers to Lebanon starting 10/1/2022
- PCR Results of Flights That Arrived on 2-1-2022
- PCR Results of Flights That Arrived on 2-1-2022
- The MoPH: Cases of COVID and Influenza Double Infection are Expected, but Not a Cause for Concern
- Ministers of Health and Education Confirm Schools and Educational Institutions Will Reopen on Monday, January 10th
- PCR Results of Flights That Arrived on 2-1-2022
- PCR Results of Flights That Arrived on 2-1-2022
- PCR Results of Flights That Arrived on 30&31-12-2021&1-1-2022
- Abiad: The Hospitals Have the Situation Under Control and We are Exerting all Efforts to Avoid Full Lockdown
- Abiad: The Increasing Number of COVID-19 Cases Shows that the Omicron Variant Is Spreading
- Lists of Psychotropic and Neurological Medication Recommended for Prescription by Specialists
- PCR Results of Flights That Arrived on 27&28&29-12-2021
- PCR Results of Flights That Arrived on 25&26-12-2021
- Ministers of Health and Interior: Omicron Variant Is Spreading and Tough Measures to Be Taken against Rule-Breakers
- PCR Results of Flights That Arrived on 24-12-2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1402/1 & 1406/1 Date 6/12/2021 & 1432/1 Date 7/12/2021
- PCR Results of Flights That Arrived on 18&19&20&21&22&23-12-2021
- Procedures For Incoming Passengers
- Maintenance on MOPH PASS Platform
- Abiad: The Lockdown Decision Will be Taken on the Basis of the Pandemic Spread
- Darwish Discussed with Abiad Ways to Support the Medical Bill
- Launch of the Awareness-Raising Campaign on COVID-19 Standards at the Tourist Facilities
- The Vaccination Campaign at Baalbek Schools Launched
- Mikati Chairs the Meeting of the Ministerial Committee for Combating the Coronavirus
- Minister Abiad: The Marathon Has Been Successful at All Levels
- Abiad Oversees the Vaccination Campaign at Zgharta Hospital
- Minister Abiad Announces his Decision on Medicine Pre-Registration
- World Antibiotic Awareness Week 2021
- PCR Results of Flights That Arrived on 11&12-12-2021
- PCR Results of Flights That Arrived on 13&14&15&16&17-12-2021
- Procedures for All Incoming Passengers to Lebanon
- Abiad: The Faster the Vaccination Campaign Goes, the Less the Possibility of Future Lockdowns
- Statement Issued by The Committee Tasked with Following up COVID-19 Preventive Measures
- Pfizer Marathon to Take Place this Weekend, Targeting all Age Groups
- Abiad Oversees the Pfizer Marathon at Batroun Hsopital
- Minister Abiad Tours the Vaccination Center at Balamand University
- Minister Abiad Visits Tripoli Hospital: Precautionary Measures Should Be Taken
- Minister Abiad: We Need to Increase the Level of Herd Immunity through Vaccination
- Abiad Starts his Tour of the North with Al-Rasi Hospital, Halba
- Abiad Visits Machghara Governmental Hospital: the Gov. Hospitals Will Have a Significant Role in the Coming Period
- Minister Abiad Visits Al Hrawi Hospital in Zahleh: the Vaccination Campaign is Excellent
- Adverse Events Following Immunization Monitoring-Covid-19 Vaccines-Lebanon
- Abiad Oversees the Marathon in Baalbek: All Support Means Will be Provided to the Hospitals and Medical Staff
- The MoPH and the Central Inspection Welcomed the European Commission’s Decision on the Vaccine Certificate of Equivalence
- Minister Abiad Visits al-Batoul Hospital in Hermel and Launches the Pfizer Marathon
- The MoPH Confirms Two Cases of Omicron Variant
- Abiad Introduced to the Donor Representatives the PHC Supportive Protocol in the Long Run
- PCR Results of Flights That Arrived on 6&7&8&9&10-12-2021
- PCR Results of Flights That Arrived on 4&5-12-2021
- Abiad and the Order of Pharmacists Head Discussed Ways to Ensure Availability and Quality of Medicines
- Abiad: Two Suspected Omicron Cases in Lebanon
- Abiad Received Medical Supplies from Brazil: a Perfect Timing
- Abiad Received a Donation of Equipment and Solar Energy Systems From Japan
- Grillo Handed over 500,000 Pfizer Vaccines to Minister Abiad
- France Donates 500,000 Doses of Pfizer Vaccines to the MoPH
- Abiad Says no Cases of Omicron Reported in Lebanon
- Third Dose Pfizer Marathon
- Volunteers Needed for the MoPH's Vaccination Campaign
- PCR Results of Flights That Arrived on 3-12-2021
- Abiad Received from the Ambassador of China the Second Batch of Medical Supplies Donation In Response to COVID-19 Pandemic
- Halabi and Abiad Oversee the Vaccination Campaign at Shakib Arslan Secondary School
- PCR Results of Flights That Arrived on 23&24&25&26&27&28-11-2021
- PCR Results of Flights That Arrived on 29&30-11&1&2-12-2021
- Minister Abiad Announced an Agreement with the World Bank to Support Hospitalization Tariffs
- Minister Abiad Visited the Laboratory for Coronavirus Diagnosis at the Lebanese University
- Minister Abiad Launched the Training Sessions on the Use of MediTrack System
- Abiad: People of all Age Groups will be Able to Get Pfizer Vaccines
- New Shipments of Medicines Delivered by the Embassy of Lebanon in South Africa Arrive in Lebanon
- Vaccination Campaign Conducted by the MoPH and the Health Committee in Collaboration with the Red Cross under Way in Hermel District
- The UNICEF Provided 97 Tons of Medical Supplies Funded by the US Government to the Lebanese Ministry of Public Health
- Proactive Measures Taken by the MoPH to Prevent Shortages of Drug Addiction Treatment
- Exceptional Approval of Hospitalization Contracts and Expenses was Granted
- The Medical Equipment and Devices Importers Syndicate in Lebanon Put Forward a Code of Conduct to Prevent Patient Rights Abuse
- Barbara Nassar Association Launched an Academy for Cancer Patients
- Ministers of Health and Social Affairs Inspected Santa Maria Elderly Care Center
- Abiad Set to Visit Santa Maria Elderly Care Center with al-Hajjar
- The Representative of Minister Abiad Participated in the Inauguration of LAU Medical Center- St John’s Hospital in Jounieh
- Minister Abiad Announced the Strategy for the Organization of the Health System
- Abiad Introduced his Plan to Address the Medicine Crisis
- The President of the Order of Nurses Visited Minister Abiad and Called for a Wage Increase
- PCR Results of Flights That Arrived on 20&21&22-11-2021
- PCR Results of Flights That Arrived on 18&19-11-2021
- The MoPH: The Seasonal Influenza Vaccine Now Available at a Subsidized Price
- Minister Abiad Declared the Termination of Contracts with Santa Maria Medical Est. And the two Medical Inspectors
- Free Medicines and a Package of Medical Services are available at the PHC Centers
- PCR Results of Flights That Arrived on 13&14&15&16&17-11-2021
- Abiad: No Total Lifting of Subsidies on Medicines for Chronic and Incurable Diseases
- Accreditation of Primary Health Care Centers in Lebanon
- Issuance of a new drugs public price list modified on 15/11/2021
- PCR Results of Flights That Arrived on 11&12-11-2021
- PCR Results of Flights That Arrived on 9&10-11-2021
- PCR Results of Flights That Arrived on 8-11-2021
- The MoPH Ensured the Transfer of Santa Maria Center Patients while Pursuing Investigation
- PCR Results of Flights That Arrived on 6&7-11-2021
- Executive Summary of the COVID 19 AEFI Report No.6
- Executive Summary of the COVID 19 AEFI Report No.5
- PCR Results of Flights That Arrived on 2&3&4&5-11-2021
- Message from the Director General Dr Walid Ammar
- PCR Results of Flights That Arrived on 1-11-2021
- PCR Results of Flights That Arrived on 31-10-2021
- PCR Results of Flights That Arrived on 29&30-10-2021
- Maternal Mental Health Guidelines for Healthcare Providers
- PCR Results of Flights That Arrived on 27&28-10-2021
- Rubella and Congenital Rubella Syndrome
- Coronavirus: invasive/novel
- PCR Results of Flights That Arrived on 26-10-2021
- PCR Results of Flights That Arrived on 22&23&24&25-10-2021
- Al-Khalil Visited Minister Abiad Who Expressed His Readiness to Deal with the Challenges Facing Hasbaya Hospital
- A Delegation of the MoPH in Akkar: the Ministry's System for Dialysis Should be Strictly Followed
- PCR Results of Flights That Arrived on 20&21-10-2021
- PCR Results of Flights That Arrived on 18&19-10-2021
- The Minister of Public Health Chairs a Meeting of Coronavirus Committee
- PCR Results of Flights That Arrived on 17-10-2021
- Research Study to Explore the Role of Government Social Media during COVID-19 Crisis
- Recommendations of the National Committee for COVID-19 Vaccine on the Administration of the Third Dose
- Warehouses Storing Missing Medicines Raided in Sad El Baouchriyeh and Tallet el-Khayyat
- The Ministry's Inspectors Seized Subsidized Medicines Stored in Ain Al Mraiseh
- PCR Results of Flights That Arrived on 14&15&16-10-2021
- PCR Results of Flights That Arrived on 12&13-10-2021
- The MoPH Requests all Hospitals to Treat the Injured at its Own Expense
- PCR Results of Flights That Arrived on 11-10-2021
- 6 People Were Killed and 32 Injured in Tayouneh Clashes So Far
- The MoPH: Death Toll From Tayouneh Clashes Rises To 7
- Minister Abiad Visits the Lebanese Order of Physicians - Beirut
- PCR Results of Flights That Arrived on 9&10-10-2021
- PCR Results of Flights That Arrived on 7&8-10-2021
- PCR Results of Flights That Arrived on 4&5&6-10-2021
- Minister Abiad Discussed with the International Committee of the Red Cross Projects to Support the Health Sector
- Four Injured in Akkar Explosion Were Received at the Airport by Minister Abiad
- Abiad Outlined the Upcoming Details of the Vaccination Plan
- Shea and Dukan Visited Abiad; The Talks Were Very Constructive, Shea
- A Delegation of the Democratic Gathering Introduced to Abiad Ways to Reinforce the Health Sector
- Abiad and the British Ambassador Discussed Projects to Support the Health Sector
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 1147/1 Date 30/9/2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1136/1 & 1137/1 & 1138/1 & 1140/1 Date 27/9/2021
- Launching of 2D Barcode Implementation on Pharmaceuticals Products and Starting the Pilot Phase in 2018
- PCR Results of Flights That Arrived on 9&10&11&12&13&14&15-9-2021
- Request for Quotation- Procurement of an Accounting Software
- Ghebreyesus Meets with the Minister of Public Health as he Visits Rafik Hariri University Hospital
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1117/1 & 1126/1 Date 10/9/2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1070/1 & 1071/1 & 1076/1 Date 10/9/2021
- MoPH Tariffs
- Outgoing Minister Hasan Handed the Ministry over to Firas Abiad
- Minister Hasan Opens an Investigation into the Death of Baby Jouri
- Hasan Calls for an Investigation into the Death of a Patient after St. Therese Hospital Denies Admission
- Minister Hasan Instructs To Open An Investigation Into The Death of A Child at Koura Hospital
- Minister Hasan Requests to Impose the Severest Penalties on anyone who Neglected the Case of the Syrian Patient
- Letter from the Minister of Public Health Addressed to the Public Prosecutor
- Closure of Two Unlicensed Drugstores in Saida
- Ministry of Health Closed a Shop in Zgharta Manipulating Food Dates and Stamping it with Red Wax
- The Moph Confirms that the Case of Fuel Storage by a Hospital Director has been Referred to the Judicial Authorities
- Minister Hasan Referred to the Justice the Case of Selling Subsidized Milk
- Minister Hasan Referred Chahine Hospital in Tripoli to the Financial Public Prosecutor's Office
- MoPH Closes Four Nurseries and Supsends their Licenses
- The MoPH Closes and Seals the Apartment of Danielle Pichon for Violating the General Health Safety Requirements
- The MoPH Calls on the Public Prosecution in Mount-Lebanon to Permanently Close Samih Al-Natour's Warehouse
- Warning Issued to Aman Medical Center in Choueifat
- A Company in Aley Closed and Sealed after the MoPH Took Action following a Complaint from Qatar
- The Moph Takes Legal Action against the Journalist Hanadi Issa for Posting a Fake Tweet
- The MoPH Continues to Carry Out Raids Targeting Warehouses Storing Medical Supplies
- Another Warehouse of Medical and Laboratory Supplies Raided in Beirut
- Minister Hasan Raided a Warehouse of Medical Supplies in Sed El Bouchrieh
- Minister Hasan Raided Warehouses of Kidney Dialysis Supplies
- Minister Hasan Receives a Letter From the State Security Following a Warehouse Raid
- Hasan Raided Unlicensed Warehouse Storing Large Quantity of Medicines in Fiyadiyeh
- A Warehouse Raided and Stored Medicines Confiscated in Toul at Midnight
- Tons of Stored Medicines Found in more than One Region
- Minister Hasan Launches Health ID
- Hasan Chairs a Meeting of the Higher Health Council to Ensure Food Safety Amid Power Cuts
- Minister Hasan Issues a Decision to Set the Dollar Exchange Rate for Unsubsidized Medicines
- Executive Summary of the COVID 19 AEFI Report No.4
- The MoPH Issues a Report on the Cases Reported among People Who Have Received Batch No. FF8111 of Pfizer Vaccine
- PCR Results of Flights That Arrived on 28&29&30&31-8&1&2&3-9-2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1032/1 Date 1/9/2021
- Hasan: The Health ID is an Achievement and Can be Used for Other Services
- Hasan Signs an Agreement Worth 1.2 M euros with the French Development Agency
- COVID-19 Testing and Vaccination Bus is now available
- All Seized Medicines and Infant Formulas to be Distributed to The Ministry's Dispensaries and PHC Centers
- Hasan Met with Members of the Importers Syndicate Council
- Hasan Chairs a Meeting to Follow up on Warehouses Inspections
- PCR Results of Flights That Arrived on 23&24&25&26&27-8-2021
- The MoPH Launches National Campaign for COVID-19 Vaccination
- PCR Results of Flights That Arrived on 21&22-8-2021
- Hasan Met with the Lebanese Pharmaceutical Importers Association
- Hasan: A Breakthrough is Achieved in the Medical Crisis
- PCR Results of Flights That Arrived on 20-8-2021
- PCR Results of Flights That Arrived on 17&18&19-8-2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.995/1 Date 18/8/2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.812/1 Date 23/6/2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.772/1 Date 14/6/2021
- Hasan: the Medicine Crisis is Close to a Solution
- Minister Hasan Expressed his Thanks to Kuwait for Evacuating 6 Injured in Al-Tleil Explosion
- The MoPH: 30 People Killed and 34 Injured Now Receiving Treatment at Hospitals Following Al-Tleil Blast
- PCR Results of Flights That Arrived on 16-8-2021
- PCR Results of Flights That Arrived on 14&15-8-2021
- Benchmark Statement Prosthetics and Orthotics Services in Lebanon
- Hasan Issues Four Emergency Import Authorizations For Lacking Medicines
- A Turkish Plane Evacuates People Injured in Al-Tleil Explosion
- PCR Results of Flights That Arrived on 10&11&12&13-8-2021
- MoPH Publishes Detailed List of Received Donations
- Minister Hasan Examines the Medicine Card Project
- Minister Hasan To Proceed with the Conclusion of Employment Contracts To Open the Turkish Hospital
- Meeting Chaired by Minister Hasan to Combine Efforts in Following up COVID-19 Cases
- A Turkish Aircraft Arrives at the Airport in Response to Al-Tleil Blast
- Hasan: An Egyptian Plane Lands in Lebanon for Medical Assistance
- The MoPH Receives a Donation of 100,000 Doses of the AstraZeneca Vaccine from Austria
- Hasan: An Egyptian Plane Lands in Lebanon for Medical Assistance
- Minister Hasan Declares a State of Emergency Following Al-Tleil Explosion
- Ongoing Contacts to Determine the Amount of Fuel Required for Hospitals
- The MoPH Explains How the Exchange Rate for Non-Subsidized Medicines Has Been Set
- The Vaccination Record Cards Issued by the Official Vaccine Platform Do not Need to be Certified
- Hasan Expects that the Drug Crisis Will be Resolved Soon
- Hasan and Kumar Jha Discuss Ways to Secure Essential Drugs for a Safe Return to Schools
- PCR Results of Flights That Arrived on 7&8&9-8-2021
- PHC Centers and Lists of Child Vaccines and Drugs for Chronic and Non-Chronic Diseases Provided by these Centers
- Minister Hasan Meets with MPs to Discuss the Durg Crisis
- Minister Hasan Considers Ways to Exchange Expertise with the AUB Regarding the Imported Medicines
- Hasan: Drug Crisis is Due to Financial Transfer
- PCR Results of Flights That Arrived on 2&3&4&5&6-8-2021
- Minister Hasan's Syrian Counterpart Says Syria is Ready to Supply Lebanon with the Medicines Needed
- PCR Results of Flights That Arrived on 30&31-7&1-8-2021
- New Procedures For All Incoming Passengers to Lebanon
- Health Minister and Industry Minister Attend Meetings in Russia
- On the One-Year-Anniversary of Beirut Port Blast, the MoPH: We Will Never Forget, You Will Never Be Forgotten
- Hasan and Hoballah Follow Up in Moscow the Preparations for the Agreement on the Production of Sputnik in Lebanon
- PCR Results of Flights That Arrived on 27&28&29&30-7-2021
- The Moph Issues Guidelines to Follow In Cases of Dog Bite, Snakebite or Scorpion Sting
- The Moph Confirms that Medicine Has been Secured to the Child Zahraa
- The Moph Calls on the Hospitals and Companies to Deliver the Medical Supplies and Implants
- PCR Results of Flights That Arrived on 25&26-7-2021
- Next Generation Sequencing Device Handed Over To the LU During a Ceremony Attended by Minister Hasan
- Hasan: The High Number of COVID-19 Cases for the Last Two Weeks is a Real Threat to Lebanon
- The MoPH Gives Permission for the Experimental Production of the Russian Vaccine
- PCR Results of Flights That Arrived on 22&23&24-7-2021
- Hasan Meets with a Delegation of the Association of Pharmacy Owners
- Minister Hasan and the Swedish Ambassador Consider Ways to Support Hospitals Damaged in Beirut Blast
- PCR Results of Flights That Arrived on 21-7-2021
- Minister Hasan Meets with a Delegation from Akroum
- The MoPH Resumes Today the Walk-in Service for Pfizer Vaccine
- The MoPH Resumes the Walk-in Service for the AstraZeneca Vaccine
- PCR Results of Flights That Arrived on 19&20-7-2021
- Minister Hasan Introduces the Ministry's Pharmaceutical Plan
- Minister Hasan Reaffirms the Ministry's Oversight Role in Dealing with Drug Shortage
- COVID-19 - Lebanon Receives another Shipment of AstraZeneca Vaccines Via Covax
- PCR Results of Flights That Arrived on 18-7-2021
- PCR Results of Flights That Arrived on 17-7-2021
- PCR Results of Flights That Arrived on 15&16-7-2021
- The MoPH: Procedures to Address the Medicine Crisis
- Minister Hasan Allows the Emergency Import and Registration of Drugs
- The Ministry of Public Health Introduces Application Forms for Exceptional Vaccination Cases
- PCR Results of Flights That Arrived on 12&13&14-7-2021
- An Announcement Issued by the Minister of Public Health, Hamad Hassan
- PCR Results of Flights That Arrived on 11-7-2021
- Temporary Freeze of Walk-In
- Hasan Stressed on the Need to Control the Medical Bill without Harming the Pharmaceutical System
- List of Primary Health Care Centers
- Minister Hasan Calls on the UN Organizations to Contribute to Drug Subsidy through the Central Bank
- Unprecedented Decision on a Mechanism to Determine the Profit Ceilings of Medical Implants
- Hasan and Caritas Consider Ways to Coordinate Efforts to Import Medicines and Infant Formula
- Minister Hasan Meets with a Delegation of the Lebanese Pharmaceutical Importers Association
- Hasan: Lebanon's Highly Skilled Healthcare Providers Protect our Society Against any Health Risks
- Open Day at the Ministry of Public Health to Find Solutions for Drug Crisis
- Central Bank Governor Informs Hasan that Bank Transfers for the Benefit of Drug Companies have just Begun
- The MoPH: the Electronic Vaccination Records Do not Need to Be Certified
- Hasan Chairs a Meeting to Draw Up a Mechanism for Contact Tracing
- PCR Results of Flights That Arrived on 5&6-7-2021
- PCR Results of Flights That Arrived on 2&3&4-7-2021
- No Vaccination Record Cards are Issued for Vaccinated People not Enrolled in the Official Platform
- Hasan Allows the Import and Registration of Drugs for Emergency Use from Different Sources
- Statement of the Central Bank Governor on the Payment of Drug Bills Following Minister Hasan's Efforts
- PCR Results of Flights That Arrived on 29&30-6&1-7-2021
- Hasan Receives a Memorial Shield from Abdul Rahman Solh in Recognition of his Humanitarian Role
- PCR Results of Flights That Arrived on 27&8-6-2021
- Minister Hasan: Lebanon Records Three Cases of the COVID-19 Delta Variant
- Hasan Met with the Parents of the Students Studying Abroad and a Delegation from the World Bank
- The MoPH Publishes a Report on the Potential Side Effects of the Vaccines
- PCR Results of Flights That Arrived on 25&26&27-6-2021
- Minister Hasan: Turkey Will Donate to Lebanon Medicines for Chronic Diseases
- Minister Hasan, MPs Trabolsy and Hossein Brought up Matters Related to the Hospitalization Sector
- Hasan and the Syndicate of Hospital Owners Discussed the New Hospital Tariff
- Adverse Events Following Immunization Monitoring-Covid-19 Vaccines-Lebanon- 14 February 2021-30 May 2021
- Minister Hasan Chairs a Meeting of the Directors of Governmental Hospitals
- President Aoun and Minister Hasan Discussed the Need to Maintain Subsidy on Medicines
- Minister Hasan Warns against the Circulation of News of Lifting Subsidies on Medicines
- Minister Hasan Examines Seized Drugs that had been Stored in an Apartment
- PCR Results of Flights That Arrived on 20&21&22&23&24-6-2021
- The MoPH Denies Issuing Statement of the First Confirmed Case of the Indian Variant
- Pfizer Marathon to Continue Tomorrow; the Number of Vaccinated People Exceeds 8500 Today
- Hasan: The Visit to Turkey Paved the Way for Cooperation in the Pharmaceutical Sector
- Grabajab.com to Book an Appointment for Pfizer Marathon and avoid Crowds
- Pfizer Marathon on June 25-26 for People aged 50 and Above
- Hasan Held Meetings during the Second Day of his Visit to Turkey
- Minister Hasan Visits the National Medicines Agency in Turkey
- Hasan and his Turkish Counterpart Consider Means of Promoting Investment in the Area of Pharmaceuticals
- PCR Results of Flights That Arrived on 17&18&19&20-6-2021
- Minister Hasan Heads to Turkey to Promote Cooperation in the Health and Pharmaceutical Sector
- Hasan Discusses Ways to Save Hasbaya Hospital from Financial Collapse
- Hasan Considers the Implementation of a Pricing Policy for the Medical Implants by a Joint Committee with the NSSF
- PCR Results of Flights That Arrived on 14&15&16-6-2021
- The Representative of the UNICEF Stressed on the Need to Strengthen Partnerships with the Ministry
- The MoPH Announces the Resumption of Reception of TB Patients at the TB Center, Karantina
- Minister Hasan Congratulates the Lebanese on Classifying Lebanon among the EU "White List"
- Hasan and a Delegation of Pharma Group Look into Ways to Secure a Donation for the Electronic Health Card
- Hasan Discusses with the Ambassador of Tunisia and the UNRWA Ways to Strengthen Cooperation
- PCR Results of Flights That Arrived on 11&12&13&14-6-2021
- Minister Hasan Signs an Agreement with the Kuwaiti Red Crescent to Secure Vaccines
- MoPH Urges the Citizens and Medical Institutions to Request Detailed Receipts for the Payments Made
- Hasan Inaugurates Lions' Kidney Dialysis Center in Bouar
- The National AIDS and Tuberculosis Control Programme Center Reopens after Reconstruction
- Hasan Chairs a Meeting of Primary Healthcare Officials
- PCR Results of Flights That Arrived on 8&9&10-6-2021
- Hasan: The Pfizer Marathon Will Take Place Every Weekend
- Hasan: We Will Reconsider the Pricing Strategy for the Medical Supplies
- The MoPH to Reduce the Age of Target Group to 53 Tomorrow
- The MoPH: Pfizer Marathon Saturday and Sunday for Residents above 55 and People with Disabilities
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.714/1 Date 31/5/2021
- Minister Hasan Inaugurates a Mega Vaccination Center, the Largest in the Country
- Hasan Chairs a Meeting and a Workshop with the Health Committee
- Pfizer Marathon this Weekend to Target Residents aged 55 and over and People with Disabilities
- Minister Hasan and the Mayors Agreed on a Mechanism to Ensure they Get Vaccinated Faster
- Pfizer Vaccine Marathon to Take Place Sunday
- PCR Results of Flights That Arrived on 3&4&5-6-2021
- Baalbek Media Forum Honors Minister Hasan
- Minister Hasan Visits Rashaya Hospital
- Hasan: Sacrifices Are Needed to Address the Difficult Situation
- The MoPH: Lebanon Classed as "Green" in France's New Travel Rulebook as Cases Decline
- Hasan Visits Zahleh Hospital: The Pfizer Marathon Will also Take Place in other Governorates
- Hasan: We Have Successfully Contained the Pandemic, the Medicine Crisis To Be Resolved Soon
- The AstraZeneca COVID-19 Vaccine is Safe and Effective
- PCR Results of Flights That Arrived on 30&31-5&1&2-6-2021
- Minister Hasan Held Talks with the World Bank Delegation
- The MoPH: the Pfizer Marathon's Launching is under Study and Will not Target People under Age 60
- Berri Met with Hasan and The Director General of the Economy Ministry
- Minister Hasan and the Turkish Ambassador Discussed Ways to Promote Mutual Cooperation
- Daher and Hasan Signed an Agreement to Secure Pfizer Vaccines for the Citizens
- Minister Hasan: Diab Was Briefed on the Central Bank's Real Figures that Should be Verified Before Publication
- World No Tobacco Day 2021
- Minister Hasan Calls for Transparency in the Pharmaceutical Sector
- Time to Register
- PCR Results of Flights That Arrived on 27&28&29-5-2021
- COVID-19 Vaccine Registration Platform
- PCR Results of Flights That Arrived on 25&26-5-2021
- PCR Results of Flights That Arrived on 27&28&29-5-2021
- PCR Results of Flights That Arrived on 23&24-5-2021
- The Implementation Procedures for "AstraZeneca Marathon"
- Minister Hasan: the Pfizer Marathon to Be Launched Soon
- Minister Hasan Concludes the Epidemiological Surveillance Program's Workshop
- Hasan: the Astrazeneca Marathon Will Take Place on a Weekly Basis
- Minister Hasan Confirmed that He Would Receive the Astrazeneca Vaccine Tomorrow
- Minister Hasan to Receive AstraZeneca Vaccine Tomorrow at the Opening of the Marathon
- Minister Hasan Visits Saint John Medical Center
- Hasan Chairs a Meeting to Draw Up an Implementation Plan for the Health Agreement Signed With Iraq
- Stored Medicines to Be Distributed Starting Tomorrow Morning under the Supervision of the Ministry
- Hasan and the Ambassador of South Korea Discuss Ways to Promote Mutual Cooperation
- Hasan Reaffirms the Central Bank's Commitment to Pay $178M for Stored Medicines
- List of the Laboratories Authorized by the Ministry of Public Health to Perform PCR Tests- 26/4/2021
- Hasan Welcomes the Decision to Pay the Amounts Due to Physicians and Hospitals
- AstraZeneca Vaccination Marathon to be Launched Saturday
- The MoPH Announces the Introduction of a Mechanism for Drug Bills and Distribution
- Minister Hasan Launched a Campaign to Vaccinate Government Employees
- PCR Results of Flights That Arrived on 22-5-2021
- Hasan and a Delegation from Kuwait Red Crescent Consider Vaccine Donation Initiative
- Hasan Commends the Sacrifices of the Palestinian People during the Session of the Council of Arab Ministers
- Arrival of 15th Shipment of the Pfizer Vaccine
- Launching of the Training Project to Enhance Performance in Hospitals
- Hasan Signs an Agreement with Makhzoumi to Secure 12,000 Doses of Pfizer Vaccines
- The MoPH's Inspection Unit Honours Dr. Badih Abou Rjaily on the Occasion of His Retirement
- PCR Results of Flights That Arrived on 20&21&22-5-2021
- PCR Results of Flights That Arrived on 18&19-5-2021
- Hasan and Bou Saab Signed an Agreement to Secure Pfizer Vaccines for the Lebanese Canadian Hospital
- PCR Results of Flights That Arrived on 16&17-5-2021
- Hasan Met with a Delegation from Civil Society Organizations to Discuss an Initiative of Solidarity with the Palestinians
- Request for Quotation of Spare Parts for CT Scan
- Adverse Events Following Immunization Monitoring-Covid-19 Vaccines-Lebanon- 14 February 2021-30 April 2021
- The Moph Plans to Widen Vaccination Scope and Clarifies the AstraZeneca Walk-ins Strategy
- Minister Hasan Met with Health Officials and Calls for an Emergency Health Plan
- PCR Results of Flights That Arrived on 13&14&15&16-5-2021
- Arrival of 13th Shipment of the Pfizer Vaccine
- Arrival of 14th Shipment of the Pfizer Vaccine
- Hasan Chairs the Meeting of the Pharmaceutical Inspectors on Subsidized Drugs and Infant Milk
- PCR Results of Flights That Arrived on 12&13-5-2021
- PCR Results of Flights That Arrived on 10&11&12-5-2021
- Minister Hasan:The Case of Ella Tannous Must Be Handled Fairly and at the Humanitarian Level
- PCR Results of Flights that Arrived on 8&9&10-5-2021
- Minister Hasan Considers Ways to Strengthen the 1214 Hotline Services
- PCR Results of Flights that Arrived on 7&8-5-2021
- PCR Results of Flights that Arrived on 5&6-5-2021
- Hasan Met with a Delegation of Beqaa Hospitals' Health Committees
- Arrival of 12th Shipment of the Pfizer Vaccine
- The Moph: People are Called to Report any Side Effects following Vaccination
- Shankiti and Minister Hasan Discussed the Strategy to Vaccinate the United Nations Staff
- Lebanon to Receive Two Million Doses of Pfizer Vaccines in June and July
- Hasan and the President of Byblos District Discussed the Role of Municipalities in Response to Vaccination Campaign
- Hasan and a Delegation from the UNICEF Examined the Preparations for the Mass Vaccination Campaign
- PCR Results of Flights that Arrived on 3&4&5-5-2021
- Hasan Met with a Delegation of the National Commission for Disability Affairs and the Social Welfare Institutions
- Hasan Chairs the Meeting of the Pharmacovigilance Committee
- PCR Results of Flights that Arrived on 1&2-5-2021
- Hasan Confirms that the Latest Figures are Encouraging and Says he will Choose to Get the Astrazeneca Vaccine
- PCR Results of Flights that Arrived on 29&30-4-2021
- Minister of Health Visits Baalbeck Governmental Hospital and Congratulates the Workers
- PCR Results of Flights that Arrived on 27&28&29-4-2021
- The Ministry of Public Health Warns against Consuming Fish of Unknown Source
- Minister Hasan Considers Setting up the Governmental Hospital Donated by Kuwait
- PCR Results of Flights that Arrived on 24&25-4-2021
- Hasan and the Union of Land Transport Look into Ways to Speed Up the Rollout of Vaccines to Drivers
- Hasan Chairs a Meeting to Outline the Mass Vaccination Campaign to Be Launched This Summer
- PCR Results of Flights that Arrived on 22&23&24-4-2021
- Arrival of 11th Shipment of the Pfizer Vaccine
- MoPH Clarifies The Reason for The Delay in The Arrival of The AstraZeneca Vaccine
- PCR Results of Flights that Arrived on 21-4-2021
- Adverse Events Following Immunization Monitoring-Covid-19 Vaccines-Lebanon- 14 February 2021-31 March 2021
- PCR Results of Flights that Arrived on 19&20-4-2021
- Hasan Receives an Invitation to Participate in the 55th Session of the Arab Health Ministers' Council
- Hasan Met with Yammine and a Delegation of the Social Security
- Hasan and Al-Majzoub Launched the Vaccination Campaign for the LU's Professors, Staff and Students
- PCR Results of Flights That Arrived on 18&19-4-2021
- Minister Hasan and the Syndicate of Pharmaceutical Industries Agreed on a Workshop to Promote Local Industry
- PCR Results of Flights That Arrived on 14&16&17&18-4-2021
- Arrival of 10th Shipment of the Pfizer Vaccine
- PCR Results of Flights That Arrived on 13&14&15-4-2021
- Hasan Considers the Building Process of Deir el Qamar Hospital with The Municipal Council
- Arrival of 9th Shipment of the Pfizer Vaccine
- Minister Hasan Signs Agreements with Several Universities to Vaccinate their Staff
- The Cuban Ambassador and Minister Hasan Discussed Lebanon's Participation in Vaccine Clinical Trials
- Minister Hasan and Musharrafieh Follow up on Lebanon's Vaccination Plan
- PCR Results of Flights That Arrived on 13-4-2021
- An Electronic Address to Help Follow up the Messages Received to Schedule Vaccination Appointments
- PCR Results of Flights That Arrived on 11&12-4-2021
- PCR Results of Flights That Arrived on 10&11-4-2021
- Request for Quotation for Procurement of Installation of Negative Pressure Systems
- Minister Hasan: We have Achieved the Maximum Possible in Spite of the Limited Vaccine Supplies
- Launching of the Vaccination Campaign for the Sinopharm Vaccine
- PCR Results of Flights That Arrived on 8&9&10-4-2021
- PCR Results of Flights That Arrived on 5&6&7&8-4-2021
- Hasan Held an Assessment Meeting with the World Bank Regional Director for the Mashreq Department
- Arrival of 8th Shipment of the Pfizer Vaccine
- PCR Results of Flights That Arrived on 4&5-4-2021
- MoPH: The Approved Vaccination Record Is the Electronic Certificate
- PCR Results of Flights That Arrived on 3&4-4-2021
- Minister's Decision No.469/1 of 1/4/2021 on the Clarification of Decision No.465/1 Regarding the Exemption of Passengers
- Request for Quotation for Procurement of Oxygen Related Equipment
- Request for Quotation for Accessories for COVID-19 Vaccine
- Request for Quotation for Accessories for COVID-19 Vaccine
- Minister Hasan and al-Hajjar Brought up the Healthcare Needs of Iqlim El Kharroub
- A Shipment of Sinopharm Vaccine Donated by the Chinese Government Arrives in Lebanon
- PCR Results of Flights That Arrived on 1/2/3-4-2021
- The Ministry of Public Health Announces The Procedures For Prioritizing People with Health Conditions for Vaccination
- PCR Results of Flights That Arrived on 1&2&3-4-2021
- Minister Hasan And His Iraqi Counterpart Signed a Framework Agreement to secure Oil in Exchange for Medical Services
- PCR Results of Flights That Arrived on 30&31-3 &1-4-2021
- Minister Hasan And His Iraqi Counterpart Tour the AUBMC and Clemenceau Medical Center
- Hasan And Al-Tamimi Visit Al-Zahraa Hospital Within the Framework of Health Cooperation Between Lebanon and Iraq
- Caretaker PM Diab Received Iraq's Health Minister and Stressed the Importance of Promoting the Cooperation Framework
- Hasan and Al-Tamimi Visit Al Rassoul Al Azam Hospital
- Minister Hasan And His Iraqi Counterpart Visit Rafik Hariri University Hospital
- Minister Hasan Signs an Iraqi Agreement
- Minister Hasan Visited AUBMC and Climeancue Hospital With Iraqi
- Minister Hasan Discussed With Tamimi the Execution of Medical Agreements
- Official Lebanese-Iraqi Discussions at MoPH
- PCR Results of Flights That Arrived on 28&29-3-2021
- Iraqi Health Minister Al-Tamimi Arrives to Beirut Airport
- Opening of Vaccination Center at Balamand University under the Patronage of Minister Hasan
- Issuance of Minister's Decision on the cancellation of PCR Tests for Travellers who Received The Covid-19 Vaccine
- PCR Results of Flights That Arrived on 25&26-3-2021
- Issuance of Memo No. 33 on 30/3/2021 on A Warning of Faking PCR Test Results
- Issuance of Memo No. 32 on 30/3/2021 on The Amendment of the Target Groups for The Covid-19 Vaccine
- Issuance of Memo No. 32 on 30/3/2021 on The Amendment of the Target Groups for The Covid-19 Vaccine
- The Moph: The Remdesivir has been Added to the Hospitalization Bill
- Hasan and the French Ambassador Consider Strengthening the Bilateral Cooperation
- PCR Results of Flights That Arrived on 27-3-2021
- The Middle East Launched the Vaccination Campaign with SPUTNIK V and Najjar the First to Get His Jab
- Minister Hasan Received a Donation from Amel Foundation
- Hasan and a Delegation of Baalbek Municipality Discussed Ways to Curb the Spread of COVID-19
- Majzoub and Hasan Launched the Vaccination Campaign for the Education Sector
- Oueidat Decides to Halt the Case Filed by Lawyers Regarding the Introduction of Iranian Drugs
- The MoPH: The Seventh Shipment of Pfizer Vaccine Arrives to Lebanon
- The Sixth Shipment of Pfizer Vaccine Arrives in the Afternoon
- Minister Hasan's Office Clarifies his Reported Statements Regarding the Russian and the Chinese Vaccines
- PCR Results of Flights That Arrived on 23&24-3-2021
- PCR Results of Flights That Arrived on 21&22&23-3-2021
- Hasan Meets with the Ambassador of Russia and Considers Purchasing One Million Doses of SPUTNIK V
- Lebanon Received 33600 Doses of The AstraZeneca Vaccine as First Batch
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.424/1 Date 23/3/2021
- World TB Day 2021
- PCR Results of Flights That Arrived on 20&21-3-2021
- Minister Hasan and Martinos Brought up the Conditions of Kartaba Governmental Hospital
- Minister Hasan and Hoballah Consider Vaccinating the Production Sector Workers
- Hasan Met with a Delegation of the General Labor Union and Announced the New Strategy for Vaccination Plan
- World TB Day 2019
- Minister Hasan and the Ambassador of Denmark Discuss Areas of Health Cooperation
- Issuance of Circular No. 14/2 on the Procedures Required by all Passengers Arriving to Lebanon
- Minister Hasan Follows up on the Establishment of Deir el Qamar Governmental Hospital
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.403/1 Date 19/3/2021
- The MoPH: The Hotlines 1214 and 1787 are Now Available Free of Charge
- PCR Results of Flights That Arrived on 17&18&19-3-2021
- Minister Hasan Announces his Iraqi Counterpart's Visit To Lebanon Next Week and a Donation from Kuwait
- PCR Results of Flights That Arrived on 16&17&18-3-2021
- PCR Results of Flights That Arrived on 14&15&16-3-2021
- The Ministry of Public Health Receives a Second Donation from the Government of Brazil
- Minister Hasan Invites Hermel Inhabitants to Register for the Vaccine
- Minister Hasan Says The Ministry will Wait before Deciding on the Use of AstraZeneca Vaccine
- PCR Results of Flights That Arrived on 13&14-3-2021
- The MoPH Has no Problem with The Private Sector's Import of Vaccines
- A New Shipment of Pfizer Vaccine Arrives in the Afternoon
- MOPH: Announcing that Vaccines are Available at High Prices will Lead to the Prosecution of the Perpetrator
- A New Shipment of Pfizer Vaccine Arrives in the Afternoon
- The MoPH Delivers five Ventilators, Drugs and Sanitizers to Brital Village
- The MoPH: The Vaccine is a National Responsibility, not a Subject of Media Hype
- PCR Results of Flights That Arrived on 12&14-3-2021
- Hasan Visits the Lebanese Canadian Hospital
- Minister Hasan Visits the National Organization for Organ Donation, Baabda
- Hasan Instructs to Open an Investigation into the Three Concurrent Deaths at the Saydet Zgharta Hospital
- PCR Results of Flights That Arrived on 6&9&10-3-2021
- PCR Results of Flights That Arrived on 10&11-3-2021
- PCR Results of Flights That Arrived on 2&3&5&6&8-3-2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.360/1 & 361/1 Date 10/3/2021
- Meeting between Minister Hasan and Hoballah in Support of the Local Manufacture of Vaccines
- Minister Hasan Requests Kumar to Increase the Number of Doses to be Received by the Ministry
- Minister Hasan Visits ECIL Center of the Imam Sadr Foundations
- Minister Hasan and Mneimneh Consider the Cooperation Association's Initiative to Secure Vaccines for The Palestinians
- Minister Hasan Honors The MoPH's Women Staff on The International Women's Day
- Minister Hasan Visits Kherbet Kanafar Governmental Hospital
- PCR Results of Flights That Arrived on 6&7&8-3-2021
- Minister Hasan Receives 30 Ventilators Donated by the African Continental Council to the Ministry
- PCR Results of Flights That Arrived on 5&6-3-2021
- The Vaccination Section at Bekaa Hospital Starts to Operate
- The UNICEF and the AFD Signed a Grant Agreement for the Renovation of Karantina Hospital's New Building
- PCR Results of Flights That Arrived on 2&3&4-3-2021
- Minister Hasan Held a Coordination Meeting on the Import of Vaccine
- PCR Results of Flights That Arrived on 1-3-2021
- Dr. Baroudi Expressed his Gratitude to Minister Hasan for his Cooperation in the Vaccination of Physicians
- The MoPH: We wasn't Duly Notified of the Interim Relief Judge's Decision
- The National Vaccination Campaign Report - From 13 to 27 February 2021
- Mental health support system for persons in quarantine
- PCR Results of Flights That Arrived on 25&27&28-2-2021
- The Ministry of Public Health Allows the Emergency Use of SINOPHARM Vaccine
- The National Vaccination Campaign Report - From 13 to 27 February 2021
- PCR Results of Flights That Arrived on 25&26-2-2021
- The MoPH: There will be no Exceptional Vaccination Campaigns
- The Ministry of Public Health Publishes a List of Private Companies that have Received Permission to Negotiate
- The MoPh: The Third Shipment of COVID-19 Vaccines Arrives in Lebanon
- PCR Results of Flights That Arrived on 24&25-2-2021
- PCR Results of Flights That Arrived on 21&22&23-2-2021
- Minister Hasan Brought Prosecution against a Man for Posing as Doctor and Inspector
- Hasan: Twenty Companies are Negotiating to Secure the Russian and Chinese Vaccines
- Minister Hasan Met with the Directors of the Accredited Vaccination Centers
- Government Controls List
- PCR Results of Flights That Arrived on 14&15-2-2021
- PCR Results of Flights That Arrived on 20&21-2-2021
- Using COVID-19 Responses to Help Strengthen the Mental Health System in Lebanon
- National Campaign to Address Stigma Related to COVID-19
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.291/1 & 292/1 Date 22/2/2021
- The Ministry's Pharmacy Inspection Committee Raided a Warehouse of Food Supplements
- Minister Hasan Raided a Warehouse of Medical Supplies being Sold at the Exchange Rate of the Lebanese Pound
- Minister Hasan Refers St.Therese and Kabr Chmoun Hospitals to Public Prosecution and Decides to Close a Medical Lab
- The MoPH: Appointments for COVID-19 Vaccines are Booked through the Official Platform
- PCR Results of Flights That Arrived on 17&18&19&20-2-2021
- Hasan: The Vaccination Campaign is Being Implemented Systematically
- PCR Results of Flights That Arrived on 16&17-2-2021
- PCR Results of Flights That Arrived on 16&17-2-2021
- Minister Hasan and the Russian Ambassador Consider Ways to Secure SPUTNIK V Vaccine
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.233/1 Date 16/2/2021
- PCR Results of Flights That Arrived on 11&13&14-2-2021
- The First Shipment of COVID-19 Vaccines to Arrive Soon
- How to Register on COVAX Platform to get the COVID-19 Vaccine
- Minister Hasan Visits Dar El Amal University Hospital in Baalbek: Vaccination will Protect the Community
- PCR Results of Flights That Arrived on 12-2-2021
- Minister Hasan Launches the Vaccination Campaigns in Baalbek and Zahleh
- Launching of Vaccination Campaign at Rafik Hariri University Hospital
- Minister Hasan Launches the Vaccination Campaign at Jesus the King Hospital, Broummana
- The First Shipment of Pfizer Vaccine Arrives to the Beirut Airport
- Minister Hasan Receives the First Batch of Pfizer Vaccine
- Ministers Hasan and Abdel Samad Visit the Vaccination Center of Saint George University Medical Center
- PCR Results of Flights That Arrived on 10&11-2-2021
- The Ministry of Public Health Announces the Arrival of the First Shipment of Vaccines
- Meeting Between Minister Hasan, World Bank Officials and the Federation of Red Cross and Red Crescent Societies
- Protective Measures against the Coronavirus
- The Ministry of Public Health Announces it had Reactivated the Hotline 1214 for any Inquiry Regarding the Vaccine
- Announcement of the Plan To Follow Up the Partial and Gradual Opening of Educational Institutions
- PCR Results of Flights That Arrived on 9-2-2021
- PCR Results of Flights That Arrived on 9-2-2021
- Minister Hasan's Media Office Denied the Vaccines had Been Distributed on the Basis of Political Preferences
- Coordination Meeting Held at the MoPH in Preparation for the Vaccination Campaign to be Launched Monday
- PCR Results of Flights That Arrived on 6&7&8-2-2021
- PCR Results of Flights That Arrived on 3&4&5&6-2-2021
- Hasan: There is no Obstacle Preventing us from Proceeding with Vaccination Campaign next Monday
- Minister Hasan Visits Jezzine Governmental Hospital
- The Moph Denies Claims of Potential Delay in the Implementation of Vaccination Campaign
- The Ministry of Public Health Allows the Emergency Use of SPUTNIK V Vaccine
- PCR Results of Flights That Arrived on 3-2-2021
- PCR Results of Flights That Arrived on 31-1-2021&1&2-2-2021
- Minister Hasan Chairs the First Meeting of the Vaccine Registration Committee
- Drugs Ethical Standards
- Clinical Trials
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.59/1 Date 12/1/2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.54/1 Date 11/1/2021
- PCR Results of Flights That Arrived on 29&30-1-2021
- PCR Results of Flights That Arrived on 27&28&29-1-2021
- PCR Results of Flights That Arrived on 27&28&29-1-2021
- Launch of the Vaccination Plan at the Grand Serail
- Ministers of Justice and Health to Take Legal and Administrative Actions against the Hospitals for Refusing Treatment
- PCR Results of Flights That Arrived on 25&26&27-1-2021
- Minister Hasan Launches a New Agreement with the World Bank to Increase the Number of ICU Beds at Governmental Hospitals
- Request for Consultancy Services for Information Technology Analyst
- PCR Results of Flights That Arrived on 24&25-1-2021
- PCR Results of Flights That Arrived on 22&23-1-2021
- The National Vaccination Plan Examined during a Preparatory Meeting Chaired by Minister Hasan
- Minister Hasan Met with MP Fatfat
- Minister Hasan and Habshi Consider Equipping the Charity Hospital in Deir el Ahmar to Receive COVID-19 Patients
- PCR Results of Flights That Arrived on 23-1-2021
- Ivermectin Donation Received by the Ministry of Public Health
- Minister Hasan Discusses with a Delegation from the UNRWA the Vaccination Plan for Palestinians
- COVID-19 Vaccine Platform to be Launched Tomorrow
- PCR Results of Flights That Arrived on 21-1-2021
- PCR Results of Flights That Arrived on 20&21-1-2021
- PCR Results of Flights That Arrived on 18&19-1-2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.87/1 & 89/1 & 90/1 Date 20/1/2021
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1896/1 Date 28/12/2020
- MOPH: The Information that has Been Spread on the World Bank Loan is Inaccurate
- PCR Results of Flights That Arrived on 17-1-2021
- The Minister of Health Inaugurates the Corona Department At Batroun Hospital
- St. George Hospital: Minister Hasan is in Good Health
- The Place of Residence of Every Person Taking The PCR Test is Required, Not Their Work Address
- PCR Results of Flights That Arrived on 16-1-2021
- PCR Results of Flights That Arrived on 16-1-2021
- PCR Results of Flights That Arrived on 14&15-1-2021
- Minister Hasan Signs the First Payment of Dues to Hospitals for the Treatment of COVID-19 Patients
- Minister Hasan Announces Berri's Initiative to Move the Field Hospital from Tyre to Beirut
- Minister Hasan Signs the Final Agreement with Pfizer
- MoPH: the Devices at the Sports City are Portable Ventilators, not ICU Ventilators
- MoPH: We Comply with Specific Standards for the Procurement of Ventilators
- PCR Results of Flights That Arrived on 10&12&13-1-2021
- St. George Hospital: Minister Hasan is in a Good Condition and is Conducting Work from Hospital Room
- PCR Results of Flights That Arrived on 12-1-2021
- St. George Hospital: Minister Hasan Tests Positive for COVID-19
- Distribution of Aid and Medical Assistance to the Hospitals following Beirut Blast on 4/8/2020
- PCR Results of Flights That Arrived on 9 & 11-1-2021
- PCR Results of Flights That Arrived on 9 & 10-1-2021
- Minister Hasan to Self-Quarantine after Three Members of his Office Staff Tested Positive for COVID-19
- Minister Hasan: The Number of ICU Beds at Private Hospitals Increased by 200
- The MoPH Launches New Hotline 1787
- PCR Results of Flights That Arrived on 27-12-2020
- PCR Results of Flights That Arrived on 26-12-2020
- PCR Results of Flights That Arrived on 22, 23, 24, 25 & 26-12-2020
- PCR Results of Flights That Arrived on 22 &23-12-2020
- PCR Results of Flights That Arrived on 18 & 19-12-2020
- PCR Results of Flights That Arrived on 16, 17 & 18-12-2020
- PCR Results of Flights That Arrived on 15 & 16-12-2020
- PCR Results of Flights That Arrived on 13 & 14-12-2020
- PCR Results of Flights That Arrived on 8&9-12-2020
- PCR Results of Flights That Arrived on 8 & 9-1-2021
- PCR Results of Flights That Arrived on 6 & 7-1-2021
- List of the Laboratories Authorized by the Ministry of Public Health to Perform PCR Tests
- Moph: The Lebanese People Need Facts that will Help them Strengthen their Confidence
- Minister Hasan Oversees PCR Testing Campaign at Fouad Chehab Stadium, Jounieh
- PCR Results of Flights That Arrived on 3-1-2021
- PCR Results of Flights That Arrived on 4&5&6-1-2021
- PCR Results of Flights That Arrived on 1&2-1-2021
- Drugs Public Price List 2020
- MoPH: Collaboration with Municipalities and Heads of Health Departments is Needed to Limit Violations
- "Ma3an" Together Against Corona
- The Cost of PCR Test at Governmental Hospitals Reduced to LBP 100,000 Starting Monday
- Hasan Decides to Downgrade the Classification of Hospitals that will not Receive Patients with COVID-19
- Hasan Addressing the Lebanese: Don't Surrender
- PCR Results of Flights That Arrived on 30&31-12-2020
- Minister Hasan Confirms that Negotiations with Pfizer will not Impact the Vaccine's Delivery by mid-February
- Closure of all Nurseries across Lebanon for the Entire Week
- PCR Results of Flights That Arrived on 29-12-2020
- National Initiative for Mental Health in the Workplace
- PCR Results of Flights That Arrived on 28-12-2020
- Minister Hasan Chairs a Meeting With the Health Inspectors
- Minister Hasan: Shutting Down the Airport is Out of the Question
- Akar, Hasan and Qatari Officials Inspect Karantina Hospital to Explore Ways to Reconstruct The Hospital
- President Aoun Gave Minister Hasan Permission to Negotiate on Securing Pfizer Vaccine
- MoPH: Pfizer Vaccine Has Been Licensed for the Emergency Use and Approved by the Ministry's Scientific Committee
- Installation of a Field Hospital in Sir Al Dinniyeh
- PCR Results of Flights That Arrived on 19&20&21-12-2020
- Minister Hasan Receives The Most Influential Figure of the Year 2020 Award
- Minister Hasan Announces the Committee's Decisions Regarding the New Corona Strain
- Minister Hasan Considers Additional Measures With the British Delegation
- Minister Hasan Opened the Corona Section at Othman Hospital in Ketermaya
- Minister Hasan Follows With MPs Hashem and Fayyad the Situations in Marjaayoun and Hasbaya Hospitals
- Request for Quotation for 5 Negative Pressure ICU - COVID19-005 - 17-12-2020
- Hasan Met With the Union of Health Mutual Funds
- Meeting on the Coverage of COVID-19 Treatment Costs by Private Insurance Companies
- Ministries of Public Health and Information Together "Ma3an" Against Corona
- Hasan Took Part In The Meeting of The New Managing Committee For Sidon Turkish Hospital
- PCR Results of Flights That Arrived on 10&11&12&13-12-2020
- WHO Technical Delegation Provides a Positive Assessment of Lebanon's Response to the Pandemic
- Minister Hasan Considers the Plan to Rationalize Subsidy with the General Labor Union
- Statement Issued by the Ministry of Health
- Bishop Darwish Visits Minister Hasan
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1685/1 & 1694 & 1695 Date 1/12/2020
- Hasan Met with the Order of the Lebanese Press Editors
- Another Batch of Seasonal Influenza Vaccines Arrives in Lebanon
- PCR Results of Flights That Arrived on 3&5&6-12-2020
- The Ministry of Public Health delivers One Hundred Thousand Masks to the Lebanese Army and The General Security
- PCR Results of Flights That Arrived on 1&4&5-12-2020
- PCR Results of Flights That Arrived on 3-12-2020
- Minister Hasan Inaugurates The Corona Department At Dar Al-Hikma Hospital
- The Expected Dates for the Arrival of Corona Vaccines in some Arab Countries
- PCR Results of Flights That Arrived on 1&2-12-2020
- Hasan: One Thousand Patients, Including Roumieh Inmates were Treated at the Expense of the WHO
- Minister Hassan Received a Delegation of the Islamic Medical Association of North Lebanon
- Minister Hassan met Al-Bustani with the Delegation of Deir Al-Qamar Hospital Committee
- Letter No.20/1/43141 of 4/12/2020 Addressed to the Governmental and Private Hospitals in Lebanon
- Inauguration of Mrayjeh Quarantine Center under the Patronage of Minister Hasan
- PCR Results of Flights That Arrived on 27&28&30-11-2020
- Announcement to all Importers and Distributors of Drugs in Lebanon
- PCR Results of Flights That Arrived on 29-11-2020
- Minister Hasan Stressed that the Ministry's Strategy to Fight the Pandemic Responds to the Global Medical Research
- PCR Results of Flights That Arrived on 28&29-11-2020
- Hassan Receives a Donation from the WHO to Governmental Hospitals and the LU
- PCR Results of Flights That Arrived on 26&27&28-11-2020
- PCR Results of Flights That Arrived on 25&26-11-2020
- PCR Results of Flights That Arrived on 23&24&25-11-2020
- Rahmeh Visits the Minister of Public Health
- Minister Hasan, Dabouq and a Delegation of Amal Movement Examined the Preparedness of Tyre's Hospitals
- The Minister of Health Met with the President of the Order of Pharmacists
- Hassan Discussed with Abdallah the Health Situation in Chouf
- PCR Results of Flights That Arrived on 21&22&23-11-2020
- Minister Hasan Chairs the Meeting of the National Committee for COVID-19 Vaccine
- PCR Results of Flights That Arrived on 21&22-11-2020
- PCR Results of Flights That Arrived on 19&20&21-11-2020
- PCR Results of Flights That Arrived on 18-11-2020
- PCR Results of Flights That Arrived on 21-11-2020
- Minister Hasan Visits Hasbaya and Rashaya Hospitals
- Hasan: Pfizer Vaccine will Arrive in Lebanon by mid-February
- PCR Results of Flights That Arrived on 18&19-11-2020
- Minister Hasan Visits the Rashid Karami Exhibition For Site Selection of the Field Hospital Funded By Qatar
- Minister Hasan Inaugurates a New COVID-19 Patient Ward at Rafik Hariri University Hospital
- PCR Results of Flights That Arrived on 17-11-2020
- Minister Hasan Chairs the Meeting of the Scientific Committee
- Minister Hasan Signs an Agreement with the Syndicate of Hospitals in Lebanon
- PCR Results of Flights That Arrived on 16-11-2020
- Joint Press Conference Between the Minister of Public Health and the Information Minister
- PCR Results of Flights That Arrived on 15-11-2020
- PCR Results of Flights That Arrived on 14&15-11-2020
- Hasan Inaugurates New COVID-19 Patient Wards In Baalbek
- PCR Results of Flights That Arrived on 11&12&13&14-11-2020
- PCR Results of Flights That Arrived on 10&12-11-2020
- PCR Results of Flights That Arrived on 11&12-11-2020
- Minister Hasan Met with Abi Ramia and was Briefed By Bakri on The Smart Health Coverage Card Project
- Protective Measures against the Coronavirus
- PCR Results of Flights That Arrived on 9&10-11-2020
- Two Qatari Planes Carrying Field Hospitals to be Set up in Tyre and Tripoli Arrive in Lebanon
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1518/1 Date 6/11/2020
- PCR Results of Flights That Arrived on 8&9-11-2020
- Memorandum Issued on the Examination of Contacts and Discharging Patients from Isolation and Quarantine
- PCR Results of Flights That Arrived on 7&8-11-2020
- Hasan Meets with the General Labor Union in Lebanon
- The MoPH Responds to the Information Disseminated on Social Media
- PCR Results of Flights That Arrived on 5-11-2020
- Hasan Inaugurates an Intensive Care Unit at Machghara Governmental Hospital
- President Aoun and Minister Hasan Raise the Issue of the Increasing Number of COVID-19 Cases
- Minister Hasan Chairs a Meeting to Assess the Mechanism Adopted by the Epidemiological Surveillance Unit
- PCR Results of Flights That Arrived on 4-11-2020
- Lists of Wealth Declarants
- PCR Results of Flights That Arrived on 2-11-2020
- Laboratory Technician Competence Exams Scheduled for Students Applying for Professional Practice License
- PCR Results of Flights That Arrived on 3-11-2020
- PCR Results of Flights That Arrived on 29&30-10 & 1&2-11-2020
- PCR Results of Flights That Arrived on 31-10&1-11-2020
- Hasan: The decree Assigning Me A Tenured Position At The Lebanese University was Issued According To The Law
- PCR Results of Flights That Arrived on 28&29&30-10-2020
- Hasan Inaugurates a COVID-19 Patient Ward at Al Rayan Hospital
- PCR Results of Flights That Arrived on 28-10-2020
- Presentation of Financial Statement - How The Grants were Received and Distributed
- Minister Hasan Visits Deir El Ahmar Medical Center
- Minister Hasan Commends the Efforts of Archbishop Darwish to Open a COVID-19 Division at Tal Chiha Hospital
- Hasan Followed the Equipping Process of a COVID-19-Specific ICU At Miniyeh Hospital
- Minister Hasan Chairs a Meeting on Ways to Implement the Twinning Program between University and Governmental Hospitals
- Minister Hasan: the Control Mechanism Adopted Contibuted to Reducing the Healthcare Bill
- PCR Results of Flights That Arrived on 24&25&26&27-10-2020
- Minister Hasan at the Groundbreaking Ceremony of Karatina Warehouse
- Hasan Inaugurates a COVID-19 Patient Ward at al Mayyas Hospital, Chtaura
- Hasan Received WHO Regional Director and Signed an Agreement with the Red Cross
- Minister Hasan Commended the Efforts of Ain Wazein Hospital
- Minister Hasan Announces that Missing Medicines will be Distributed as from Tomorrow
- Minister Hasan Raids a Warehouse of Medicines in Dbayeh
- PCR Results of Flights That Arrived on 24-10-2020
- Meeting between Minister Hasan and the Orders of Phsicians on Children's Vaccination
- Hasan and Samadi Consider Proceeding with Sidon Governmental Hospital Setup
- Minister Hasan Chairs the Meeting of the Scientific Committee
- Minister Hasan Inaugurates Imam Al Sader Quarantine Facility in Arabsalim
- PCR Results of Flights That Arrived on 23-10-2020
- Minister Hasan: BDL's Statement Reassuring
- Minister Hasan Examines Mays El Jabal Hospital's Scanning Device Donated by the Assocation of Banks to the Ministry
- PCR Results of Flights That Arrived on 22&23-10-2020
- PCR Results of Flights That Arrived on 21-10-2020
- PCR Results of Flights That Arrived on 20-10-2020
- Minister Hasan Visits Bayt Lif Hospital
- Minister Hasan Inaugurates a COVID-19 Patient Ward at Ragheb Harb Hospital
- PCR Results of Flights That Arrived on 17&19-10-2020
- Monitoring of COVID-19 Infection In Lebanon -21/10/2020
- Hasan Discussed with a Delegation of the Strong Lebanon Bloc the Health Implications of Beirut Blast
- Monitoring of COVID-19 Infection In Lebanon -21/10/2020
- MoPH: Unofficial PCR Test Results were Sent to the Citizens
- Minister Hasan Discussed with the Newly Appointed Russian Ambassador Ways to Strengthen Health Cooperation
- Minister Hasan Requests President Aoun to Exempt the Health Sector from BDL's Latest Circular
- PCR Results of Flights That Arrived on 18-10-2020
- PCR Results of Flights That Arrived on 16&17&18-10-2020
- Minister Hasan Chairs a Meeting to Ensure Provision of Medicine
- Statistics 2019
- Statistics 2019
- PCR Results of Flights That Arrived on 15&16-10-2020
- Hasan: Any Hospital That Dedicates Intensive Care Units Will Benefit From Ventilators
- Hasan: The Claim That A University Hospital Rejected Veiled Students Was Unfounded
- PCR Results of Flights That Arrived on 14&15-10-2020
- The Advisor To The Minister Rejects Claims That The Test Results of The Passengers Arriving From Najaf Were Inaccurate
- PCR Results of Flights That Arrived on 12&13&14-10-2020
- Minister
- Minister Hasan Visited a Drug Warehouse in Baabda
- Shutdown of Pharmacies in Zahleh for Drug Smuggling
- PCR Results of Flights That Arrived on 11&12-10-2020
- The Moph Launches the Second Round of Vaccination Campaign in Collaboration with UNICEF and WHO
- Minister Hasan: The Situation in Lebanon is Alarming
- Minister Hasan Received a Delegation of the General Labor Union
- Decisions of the Minister of Public Health to Close Three Pharmacies
- Minister Hasan Chairs The Meeting of The Scientific Committee
- Minister Hasan Participated in the 67th Session of the WHO Regional Committee
- PCR Results of Flights That Arrived on 10&11-10-2020
- Hasan Launches The New Technique For The Diagnosis of COVID-19 Infection
- PCR Results of Flights That Arrived on 10-10-2020
- Minister Hasan, al-Jisser and Tripoli Hospital's Director Follow up on the Efforts to Increase the Number of ICU Beds
- Minister Hasan Chairs A Meeting On Drug Crisis And Takes A Decision to Close Two Pharmacies
- Minister Hasan Inaugurates A Corona Virus Ward At Rayak Hospital
- PCR Results of Flights That Arrived on 9&10-10-2020
- PCR Results of Flights That Arrived on 8&9-10-2020
- PCR Results of Flights That Arrived on 6&8-10-2020
- PCR Results of Flights That Arrived on 6&7-10-2020
- PCR Results of Flights That Arrived on 5&6-10-2020
- Support to Integrated Service Provision at the Local Level in Coordination with UNDP
- Request for Expression of Interest- 8/10/2020
- PCR Results of Flights That Arrived on 4&5-10-2020
- Hasan and Moussa Brought up the Situation in Prisons as COVID-19 Cases Surge
- National action plan for the mental health and psychosocial support response to Beirut Explosion Disaster
- Minister Hasan Announces a Plan to Increase the Number of Beds in the Governmental Hospitals
- Hasan and a Russian Delegation Discussed Ways to Secure the Russian Vaccine once Approved
- Minister Hasan Met with Hajjar, Abdallah and a Delegation of Siblin Hospital
- The Lebanese Pharmaceutical Importers Suspsended the Decision of Halting the Delivery of Medical Supplies
- Memorandum Issued by the Minister on the Mechanism for the Use of Influenza Vaccine
- PCR Results of Flights That Arrived on 3&4-10-2020
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1352/1 and 1359/1 and 1360/1 and 1361/1 Date 2/10/2020
- Hasan and Kanaan Discussed the Budget of the Ministry of Public Health
- Minister Hasan Met with Representatives of University Hospitals
- Hasan Met with Ohanian and Pakradounian
- Minister Hasan: Infection Rate Draws Lebanon Closer to Europe's Scenes
- Minister Hasan: We are Seeking to Increase the Number of ICU Beds
- Statement Issued by the Ministry of Public Health Concerning the Investigation in Alleged PCR Results
- Minister Hasan Visits Dar al Amal Hospital
- MOPH Teams Start to Conduct Surveys for Contact Tracing and Indicator Issuance in Areas under Lockdown
- Minister Hasan Received a Designer of a Smart Stick for the Visually Impaired People
- Minister Hasan Offered his Condolences for the Passing of the Late Emir of Kuwait
- PCR Results of Flights That Arrived on 2&3-10-2020
- PCR Results of Flights That Arrived on 1&2-10-2020
- PCR Results of Flights That Arrived on 1-10-2020
- PCR Results of Flights That Arrived on 29&30-9-2020
- Hasan Signs an Agreement according to which the LU Performs PCR Tests for Passengers at the Airport
- Extended Meeting at the MOPH and Agreement on the Tariffs of PPE
- Minister Hasan Meets with the Chargé d'Affaires of the Iraqi Embassy in Lebanon
- PCR Results of Flights That Arrived on 28&29-9-2020
- PCR Results of Flights That Arrived on 27&28-9-2020
- PCR Results of Flights That Arrived on 26&27-9-2020
- Minister Hasan Visits the Central Drug Warehouse Damaged by the Explosion
- Fadi Saad Presented to Minister Hasan a Study Confirming a Drug's Effectiveness in Reducing COVID-19 Deaths
- Coordination Meeting to Activate Cooperation between MoPH and MSF
- PCR Results of Flights That Arrived on 26-9-2020
- Minister Hasan in Qobeiyat: COVID-19 is still Spreading and we Should not Underestimate its Risks
- 16 Positive Cases among the Passengers on Flights to Beirut in the Last Two Days
- MOPH: PCR Tests are not Available for Free for Everyone at the Italian Field Hospital
- Hasan in Bebnine: We are Working Hard to Increase the Number of Beds for COVID-19 Patients
- Minister Hasan Visits Fnaydek: The Cooperation of Local Community Leads us to Safety
- Awareness-Raising Event in Bsharreh to Overcome COVID-19
- Hasan Arrives in Qobeiyat and Meets with the Crisis Cell
- The Ministry of Health Denies Incorrect Information on the Drugs Application
- PCR Results of Flights That Arrived on 23&24-9-2020
- Minister Hasan and the President of the Pharmacists' Syndicate Consider Ways to Rationalize Drug Prescription
- PCR Results of Flights That Arrived on 21&22&23-9-2020
- Minister Hasan Chairs a Meeting to Assess the Measures Taken at the Airport
- PCR Results of Flights That Arrived on 20 & 21-9-2020
- Minister Hasan Met with Hasan Ezzeddine on the Equipment of Kana Governmental Hospital
- PCR Results of Flights That Arrived on 20 & 21-9-2020
- Minister Hasan Announces the Recommendations of the Scientific Committee
- Minister Hasan Chairs the Meeting of the Specialists' Committee for the Regulation of Laboratories Authorization
- PCR Results of Flights That Arrived on 19-9-2020
- Issuance of Two Decisions on the Implementation of the Barecode on Drugs
- Minister Hasan Visits al-Shifa Hospital in Aramoun
- Minister Hasan Tours the Psychiatric Hospital of the Cross
- Minister Hasan and UNICEF Representative Consider Ways to Support Lebanon to Join GAVI
- PCR Results of Flights That Arrived on 18&19-9-2020
- PCR Results of Flights That Arrived on 17&18-9-2020
- PCR Results of Flights That Arrived on 16&17-9-2020
- Minister Hasan's Intervention on Health Sector Challenges
- PCR Results of Flights That Arrived on 15&16-9-2020
- PCR Results of Flights That Arrived on 13&14&15-9-2020
- PCR Results of Flights That Arrived on 13&14-9-2020
- Minister Hasan Chairs a Meeting on Pharmaceutical Issues and Securing COVID-19 Vaccine
- Minister Hasan Looks into the Possibility of Completing Bsharreh Hospital's Rehabilitation
- Minister Hasan Chairs a Meeting to Draw up a Response Plan for Prisons
- PCR Results of Flights That Arrived on 13&14-9-2020
- Minister Hasan Received a Delegation of Serum Factories
- Thank you from the Heart Message from Minister Hamad Hassan
- Minister of Public Health: Coronavirus is a Tough Reality and a Real Danger
- PCR Results of Flights That Arrived on 12-9-2020
- Minister Hasan Inaugurates a Coronavirus Division at Bar Elias Hospital
- PCR Results of Flights That Arrived on 11&12-9-2020
- PCR Results of Flights That Arrived on 11-9-2020
- Preventing suicide in Lebanon-Much can be done with whole-of-society approach
- PCR Results of Flights That Arrived on 10&11-9-2020
- Minister Hassan Opened The Corona Center At Qana Hospital
- PCR Results of Flights That Arrived on 9&10-9-2020
- Hemodialysis Patients with COVID-19 in Lebanon
- PCR Results of Flights That Arrived on 6 & 7 & 8 - 9 - 2020
- PCR Results of Flights That Arrived on 9-9-2020
- Minister Hasan Discussed with Sherri and Moussawi the Health Situation and Pharmaceutical Matters
- Minister Hasan Received Dr Maroun Khoury: Health Strategy in Response to COVID-19 Achieved Positive Results
- Minister Hasan Visits the Italian Field Hospital at the Lebanese University, Hadath
- Ministers Al Samad and Al Mokdad Visit Minister Hasan
- PCR Results of Flights That Arrived on 8-9-2020
- The Ministry of Public Health Launches "Ma3an" the Mobile Application for Contact Tracing
- PCR Results of Flights That Arrived on 6-9-2020
- Hasan Visits The Epidemiological Surveillance and Hotline Centers
- Hasan and Yammine Discuss Ways to Fight Pandemic In Zgharta District
- PCR Results of Flights That Arrived on 4&5&6-9-2020
- Minister Hasan Hands over A PCR Expert Device to Ehden Governmental Hospital
- The Minister of Health Held A Meeting In Tripoli to limit the Spread of Corona
- PCR Results of Passengers That Arrived on 3&4&5-9-2020
- Minister Hasan Expressed his Gratitude to his Egyptian Counterpart for the Support to the Lebanese Health Sector
- Additional PCR Results of Flights That Arrived on 3&4-9-2020
- PCR Results of Flights That Arrived on 3&4-9-2020
- Ministry of Health: Quarantine is Mandatory for Those In Contact with Positive Cases Throughout the Incubation Period
- PCR Results of Flights That Arrived on 2&3-9-2020
- The Minister of Health Sets the Addresses of Support for Private Hospitals
- The Minister of Health Discussed With the President of Beirut Arab University the Accreditation of Its Laboratory to Conduct Medical Tests
- Updated List of the Names of the Beirut Port Explosion Martyrs
- Minister Hasan: the MoPH to Cover the Treatment Costs of the Injured
- Minister Hasan: We Keep our Promise with ongoing Efforts towards the Development of the Health Sector
- PCR Results of Flights That Arrived on 31-8 & 2-9-2020
- PCR Results of Flights That Arrived on 1&2-9-2020
- MoPH: Free Health Care Services are Provided to Patients at the Field Hospitals
- List of Field Hospitals That Treat Patients For Free
- Minister Hasan Received a Donation of Medicines from his Egyptian Counterpart
- PCR Results of Flights That Arrived on 31-8-2020 and 1-9-2020
- A Cooperation Agreement Between the MoPH, WHO, and Saint Joseph University to use Academic Expertise
- Lebanese Health Minister and his French Counterpart Oversaw a Trial of Detection Dogs at the Airport
- PCR Results of Flights That Arrived on 30&31-8-2020
- PCR Results of Flights That Arrived on 29 & 30-8-2020
- Minister Hasan, Nahas and Darwish Discussed the measures to be taken to face the growing number of infections in North Lebanon
- Hassan Chaired the Meeting of the Scientific Committee and Warned That Corona Is Not A Lie
- Hassan Announced The Distribution of A Contribution of 15 Billion Lira to 10 Governmental Hospitals
- PCR Results of Flights That Arrived on 29 & 30-8-2020
- Meeting of the National Infectious Disease Committee on 24/8/2020
- PCR Results of Flights That Arrived on 27 &28 &29-8-2020
- PCR Results of Flights That Arrived on 26 &27 &28-8-2020
- Clarification from the Ministry of Public Health Regarding the Tests Conducted in Qubb Elias
- PCR Results of Flights That Arrived on 26&27-8-2020
- Minister's Office Denies the Infection of the Work Team with Covid-19
- Hassan Opened the Corona Department at Al Zahra Hospital
- PCR Results of Flights That Arrived on 25&26-8-2020
- Minister Hasan Inspects Oyoun Samak Lake
- Minister Hasan Visits Microbiology Health and Environment Laboratory, Tripoli
- Minister Hasan Visits Abboudiyeh Border Crossing Point
- Minister Hasan Inspects the Fire Damages to Orange Nassau Hospital,Tripoli
- Minister Hasan Announced the Start of the Reception of Corona Patients At St. George's Hospital-Hadath
- PCR Results of Flights That Arrived on 25-8-2020
- Cooperation Protocols Signed by and between the Governmental Hospitals and the Lebanese University
- HOW TO SUPPORT SOMEONE AFTER A TRAUMATIC EVENT- TIPS BASED ON PSYCHOLOGICAL FIRST AID
- HOW TO HELP CHILDREN COPE WITH A TRAUMATIC EVENT
- Tipsheet- for OBYN and Midwives following Beirut Explosion
- Directory of mental health professionals for mental health support for persons affected by Beirut explosion
- National Mental Health and Psychosocial Support Response to Beirut Explosion
- PCR Results of Flights That Arrived on 24 & 25-8-2020
- PCR Results of Flights That Arrived on 22-23 & 24-8-2020
- Minister Hasan Toured Chehar el Gharbi Hospital Yesterday Evening
- Minister of Youth and Sports and Minister of Public Health Visit Atwi at al Makassed Hospital
- Saint Georges Hospital to Start to Admit Coronavirus Patients Next Week
- Minister Hassan Receives 6 Ventilators as a Donation to be Distributed to Hospitals
- The Ministers of Health and Information Discuss in a Joint Conference the Second Wave of the Epidemic
- Opening of the Center For The Distribution of Medicines For Incurable Diseases
- Minister Hasan Receives from the Ambassador of India the Second Donation of Medical Supplies
- Hasan Receives Tlais and the Health Official of Amal Movement
- Minister Hasan Oversees Rehabilitation Work at Wardieh Hospital
- Minister Hasan and Abdallah Discussed the Health Situation in Iqlim El Kharroub
- Minister Hasan Met with the Medical Mission from Kazakhtan that Followed up the Treatment of the Injured
- PCR Results of Flights That Arrived on 22-8-2020
- PCR Results of Flights That Arrived on 21-8-2020
- Minister Hasan Explains The Strategy To Address The Covid-19 Epidemic
- Health Minister's Fabricated Account on Twitter
- Hasan: The Families of the Patients who Die from COVID-19 shall not Receive any Compensation
- MoPH: Calling into Question some Lab Results would not be in the Public Interest
- PCR Results of Flights That Arrived on 20-8-2020 and 21-8-2020
- The Ministry of Health Was Surprised By The Claim That It Was Charging Money For Corona Patients
- PCR Results of Flights That Arrived on 20-8-2020
- PCR Results of Flights That Arrived on 19-8-2020 and 20-8-2020
- Minister Hasan Supervised The Final Trials of Trained Dogs To Detect Virus At Airport
- Minister Hasan and the Ambassador of Egypt Inspect the Healthcare Center of the Arab League
- MoPH Media Office Issued General Mobilization Instructions
- PCR Results of Flights That Arrived on 18-8-2020 and 19-8-2020
- Hasan and Okais Brought up the Health Situation in Zahleh District as COVID-19 Spreads
- PCR Results of Flights That Arrived on 16-8-2020 and 17-8-2020 and 18-8-2020
- PCR Results of Flights That Arrived on 16-8-2020 and 17-8-2020
- The Health Committee Submitted its Recommendation of a two-Week Lockdown
- Minister of Public Health and Minister of Public Works Inspect Notre Dame de Secours Hospital
- PCR Results of Flights That Arrived on 16-8-2020
- Minister Hasan Calls for a Two-Week General Lockdown
- Minister Hasan Chairs a Meeting of the National Committee for the Use of Dogs to Detect COVID-19 Cases
- PCR Results of Flights That Arrived on 15-8-2020
- Minister Hasan Called Berri and Agreed with Araji to Hold a Meeting of the Health Committee Tomorrow
- Minister Hasan: We have Started to Isolate some Neighborhoods in Many Regions
- Road Map for the Operation of Trauma and Emergency Hospital in Sidon
- Minister Hasan and the Representative of Erdogan Inspects the Turkish Trauma and Burn Medical Center in Sidon
- Additional PCR Results of Flights That Arrived on 14-8-2020
- PCR Results of Flights That Arrived on 14-8-2020 and Additional Results of Flights on 12-8-2020 and 13-8-2020
- PCR Results of Flights That Arrived on 13-8-2020 and Additional Results of 11-8-2020
- Additional PCR Results of Flights That Arrived on 12-8-2020
- Minister Hasan Asked Customs to Report on Expired Drugs
- Minister Hasan Signs a Cooperation Agreement with the Swiss Ambassador for the Rehabilitation of Saint George and Quarantine Hospitals
- PCR Results of Flights That Arrived on 12-8-2020 and Additional Results of 10-8-2020 and 11-8-2020
- The Office of the MoPH Issues a Statement Regarding the Coverage of a Child's Special Treatment
- Minister Hasan Received a Medical Aid from Tunisia
- Minister Hasan and the Moroccan Ambassador Inspect the Field Hospital Funded by Morocco
- The Media Office of the MoPH Denies Claims that it Refused to Treat the Injured at its Expense
- President Aoun Chairs a Meeting on the Urgent Measures to be Taken to Curb the Spread of COVID-19
- Minister Hasan Visits St. Joseph Hospital, Dora
- Minister Hasan and a Turkish Delegation Consider Ways to Begin Operating the Emergency Hospital in Sidon
- PCR Results of Flights That Arrived on 10-8-2020 and Additional Results of Flights on 8-8-2020 and 9-8-2020
- Drugs Public Price List 2019
- Re-Opening of the Drug Distribution Center in Karantina
- Minister Hasan Considers Proceeding with the Implementation of the Agreement with the Lebanese University
- The Envoy of Belgium's Reformist Movement Party Expressed her Condolences to Minister Hasan
- Minister Hasan Chairs the First Meeting of the Commission to Study the Impacts of Beirut Blast on Health and Environment
- Hasan and WHO Emergency Director Raised the Issue of Growing Challenges
- PCR Results of Flights That Arrived on 9-8-2020 and 8-8-2020
- Minister Hasan Discussed with a Delegation of the EU Ways to Facilitate Access to Medical Assistance
- Minister Hasan Met with the Ambassador of Japan
- Minister Hasan Proposed that some Regions be Isolated Due to COVID-19 Spread
- The Ministry of Public Health Issues a List of the Names of the People Killed in Beirut Blast
- The Ministry's Refusal to Treat the Injured at its Expense: a Baseless Claim
- Hasan Tours Zahleh: Lockdown to be Imposed on a larger Scale as Covid-19 Cases Increased
- Minister Hasan Visits Hallaniya: I will Propose that a State of Emergency be Declared in some Districts
- Ministry of Public Health: 158 Dead, more than 6000 Injured and 21 Missing
- PCR Results of Flights That Arrived on 8-8-2020
- PCR Results of Flights That Arrived on 7-8-2020
- Additional PCR Results of Flights That Arrived on 7-8-2020
- PCR Results of Flights That Arrived on 6-8-2020
- Meetings with the Minister of Public Health Dr Hamad Hasan
- PCR Results of Flights That Arrived on 5-8-2020
- A Statement Issued by the Ministry of Public Health
- Minister Hasan: The Number of Victims of Beirut Explosion Rose to 154
- PCR Results of Flights That Arrived on 4-8-2020
- Minister Hasan Expects an Increase of COVID-19 cases
- The Minister of Health Visits Karantina Hospital
- Minister Hasan Visits the Injured at the AUBMC
- Minister of Health Inspects Iran's Field Hospital at Hadat
- Hasan and Ohanian's Visit to the Russian Field Hospital
- List of the Names of all the Victims whose Bodies are at the Governmental Hospitals
- Minister Hasan Instructs Hospitals to Treat the Injured at the Ministry's Expense, upon the Directives of Prime Minister Diab
- The MoPH Calls on the Medical Teams to Volunteer and Launches a Hotline for the Treatment of Injured
- Circular Issued by the Minister of Public Health on the Mechanism for Detecting Cases on the Borders
- Additional PCR Results of Flights That Arrived on 1-8-2020 and 2-8-2020
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.976/1 Date 23/7/2020
- PCR Results of Flights That Arrived on 30-7-2020 and 31-7-2020
- Moph: The Hospitals are Bound to Admit all the Patients, Including the Suspected Cases
- Minister Hasan Announces that Heads of Hospitals are Summoned for Investigation
- PCR Results of Flights That Arrived on 1 & 2-8-2020
- Meeting of the National Infectious Disease Committee on 29/7/2020
- Minister Hasan Mourns Nurse Zaynab Haydar
- Hasan Met with the Owners of the Laboratories Qualified to Conduct PCR Tests
- Hasan Discussed with the Insurers Ways to Strengthen Coordination
- Additional PCR Results of Flights That Arrived on 30-7-2020 and 31-7-2020
- PCR Results of Flights That Arrived on 29-7-2020 and 30-7-2020
- PCR Results of Flights That Arrived on 29-7-2020
- PCR Results of Flights That Arrived on 28-7-2020
- PCR Results of Flights That Arrived on 12-7-2020
- PCR Results of Flights That Arrived on 11-7-2020
- PCR Results of Flights That Arrived on 27 & 28-7-2020
- Minister Hasan Visits Tannourine Governmental Hospital
- Minister Hasan to Visit this Evening Hellaniya where Cases have been Reported before Heading to Saraain
- Hasan visits Bassil in Batroun
- PCR Results of Flights That Arrived on 14-7-2020
- PCR Results of Flights That Arrived on 15-7-2020
- PCR Results of Flights That Arrived on 17-7-2020
- PCR Results of Flights That Arrived on 18-7-2020
- Additional PCR Results of Flights That Arrived on 20-7-2020
- PCR Results of Flights That Arrived On 10-7-2020
- PCR Results of Flights That Arrived on 13-7-2020
- PCR Results of Flights That Arrived on 16-7-2020
- PCR Results of Flights That Arrived on 21-7-2020
- PCR Results of Flights That Arrived on 19-7-2020 and 18-7-2020
- PCR Results of Flights That Arrived on 22-7-2020
- PCR Results of Flights That Arrived on 23 & 24-7-2020
- PCR Results of Flights That Arrived on 23-7-2020
- PCR Results of Flights That Arrived on 24 & 25-7-2020
- PCR Results of Flights That Arrived on 25 & 26-7-2020
- PCR Results of Flights That Arrived on 26 & 27-7-2020
- PCR Results of Flights That Arrived on 5-7-2020
- PCR Results of Flights That Arrived on 6/7/2020
- PCR Results of Flights That Arrived on 7/7/2020
- PCR Results of Flights That Arrived On 8-7-2020
- PCR Results of Flights That Arrived On 9-7-2020
- PCR Results of Passengers That Arrived on 1/7/2020 and 2/7/2020
- PCR Results of Passengers That Arrived on 2/7/2020
- PCR Results of Passengers That Arrived on 3/7/2020
- Minister Hasan Inaugurates a Section for the Treatment of Patients with COVID-19 at al-Rassi hospital
- Monitoring of COVID-19 Infection In Lebanon - 14/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 7/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 8/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 10/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 13/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 17/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 20/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 5/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 6/5/2020
- Monitoring of COVID-19 Infection In Lebanon - 9/4/2020
- Minister Hasan Presents the Indicators of the Worsening Situation
- Minister Hasan and Sarraf Raised the Question of Establishing a Military Hospital in Akkar
- Minister Hasan Announces the Recommendations of the Scientific Committee
- Minister Hasan Visits Baalbeck Governmental Hospital: We Have Reached a Dangerous Turning Point
- Hasan Visits the Injured Passenger following the Iranian Plane Incident
- Ali Ammar Visits Minister Hasan: Citizens Should Comply with the Preventive Measures
- Minister Hasan and Haroun Brought up the Challenges to the Hospitalization Sector
- Minister Hasan Visits Baabda Governmental Hospital
- A Delegation of the Ministry Offers Condolences to the Family of Doctor Ismail
- Minister Hasan Visits Dahr el Bachek Hospital in the Presence of Kanaan
- Health Minister and Industry Minister Tour the Serum Factory in Choueifat
- Health Minister and Industry Minister Visit a Pharmaceutical Factory in Jadra
- MoPH Mobile Applications
- Issuance of Circular No. 99 About Travelers Coming To Lebanon
- Minister Hasan and the ISF Director General's Representative Launched The New Detection Method Using Trained Dogs
- Events
- Minister Hasan Launches "Ma3an-Together against Corona" Application
- Workshop at the Ministry on the Use of the Information System for the Service of the Incoming Passengers
- Workshop on Virtual Consultation for Volunteer Doctors
- The General Mobilization: How Long Will It Last?
- Minister Hasan Launches MoPH Chatbot on WhatsApp
- Minister Hasan Launches MoPH Chatbot on WhatsApp With an Initiative From the Lebanese University Students
- Cooperation Agreement Between Mount Lebanon Hospital and University of Balamand
- Minister Hassan Follows up with the Epidemiological Surveillance and the Call Center
- Meeting Between Minister Hasan and Head of UNFPA Office In Lebanon on the Framework of Cooperation
- Training of Volunteers to Support Quarantined Citizens to Use MoPH’s Digital Platforms And Facilitate Follow up Procedures
- Article publié dans "L'Orient Le Jour" sur l'importance du site éléctronique du Ministère
- Minister Hasan Chairs A Meeting with The Health Inspectors As Part of The Ongoing Food Safety Program
- Coronavirus COVID-19 Lebanon Cases
- Workshop for the Medical Personnel on the Preventive Measures and for the Hotline Team
- Jabak and the WHO Launched the Lebanon Clinical Trials Registry (LBCTR), the First of its Kind in the Arab Countries
- Launching of EHealth Lebanon Mobile App. for MoPH Digital Services
- On the Launching of the Pilot Phase for the New Emergency Plan within 2025 Strategy Hasbani: The financial Ceilings were Set for the First Time according to a Scientific and Practical Mechanism
- Launching of Citizens Right Project
- Hasbani Launched a New Mobile Application that Makes every Citizen a Partner in the Health Control Process
- Signature of a Memorandum of Understanding between the Ministry of Public Health and the Lebanese Customs to Launch the e-Signature of Customs Declaration
- Health Minister Receiving Smart Government Award
- Launching of the One Stop Shop for Administrative Procedures in Presence of OMSAR Minister
- Launching of the New Version of the MOPH's Website and E-Services Platform
- Golden Excellence Award for the Lebanese Ministry of Public Health - Kuwait 2016
- Best Smart Mobile Application Award for the Lebanese Ministry of Pubic Health- Kuwait 2015
- MOPH Mobile Application
- E-Government Web Awards
- PCR Results of Flights That Arrived on 20-7-2020
- Lebanese Customs Raided 3 Warehouses of Spoiled Chicken in Zekrit
- Minister Hasan Receives a Donation of Face Masks
- Minister Hasan Receives a Donation of Face Masks
- Minister Hasan Considers the Adoption of COVID-19 Early Diagnosis Method using Trained Dogs
- Two Labs for PCR Tests Granted by the International Atomic Energy Agency
- Minister Hasan Met with a Delegation of Midwives
- Minister Hassan Discussed With Al-Ahed to Host the First Group in the Asian Cup Qualifiers
- Minister Hasan Announces That Stricter Measures Will Be Taken To Avoid Community Transmission
- Issuance of Memorandum No.107 of 17/7/2020 by the Minister on the extension of the period of barcode implementation
- Minister Hasan Receives a Memorandum of Claims from the Syndicat des Opticiens et Optometristes
- Meeting between the Minister of Public Health and the Italian Ambassador on the Joint Cooperation Programs
- Minister Hasan Chairs a Meeting to Step up the Measures against COVID-19
- Suppressing COVID-19 Transmission 19/7/2020
- Hassan Chaired the Scientific Committee Meeting at MoPH
- Lebanon Health Resilience Project in Collaboration with the World Bank
- test
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.919/1 Date 13/7/2020 and 955/1 Date 14/7/2020
- The Ministry's 1214 Hotline Services Suspended
- Minister Hasan Offers Condolences to the Family of the Child who Died at Tripoli Hospital
- Ministry of Health Announced The Follow Up of The PCR Results of Incoming Passengers
- Minister Hasan: We Need to Cooperate to Face the Increasing Number of COVID-19 Cases
- Diab Chaired a Meeting of the Coronavirus Follow-up Committee
- Minister Hasan: Some Vaccines Require a Close Cooperation according to the Law
- Minister Hasan Chaired a Meeting for the Ministry Officials with the Acting Director General
- Minister Hasan Chairs a Committee's Meeting on the Preventive Measures to Curb the Spread of COVID-19
- Zeaiter Following his Meeting with Minister Hasan: The Situation is not Alarming, but Precautions must be Taken
- PCR Tests Administered to Contacts of Confirmed Cases in 4 District Villages
- Minister Hasan Visits Baalbeck: We are Facing the Challenge of Expat Repatriation
- The Minister of Public Health Follows up the Process of Equipping the Governmental Hospitals
- Minister Hasan Looks into Solutions to the Challenges facing the Dentists
- Minister Hasan Sponsored the 23rd Congress of the Lebanese Society of Endocrinology, Diabetes and Lipids
- Joint Press Conference between Health Minister, Education Minister and LU President
- Minister Hasan and Mokdad Brought up the Problems of the Health Sector
- A Medical Team from the Ministry Performed 230 PCR Tests in Jeddayel and Neighboring Towns
- The Ministry of Public Health was Handed out PPE in Aid from Brazil
- Minister of Public Health and Minister of Industry Toured Pharmaline Pharmaceutical Company
- Minister of Public Health and Minister of Industry Visited Benta Industries in Dbayeh
- Hasan Met with the New President of Doctors Without Borders
- Minister Hasan's Interview With Tele Liban
- Minister Hassan Held a Video Conference With 5 Governmental Hospitals
- Hasan Takes Part In A Seminar Organized By ESCWA on The Rate of COVID-19 Infections
- Minister Hassan and the Council of the Order of Pharmacists Brought Up the Issues of the Sector
- Minister Hasan Received The Iranian Ambassador
- Meeting of the National Infectious Disease Committee on 6/7/2020
- Minister Hasan Toured Health Centers in Nabatieh
- MoPH: One Positive Case Friday and two other Infections Saturday among the Returning Passengers
- Minister Hasan Oversaw the Preparations for Baalbeck Concert
- Health Minister and Information Minister Followed up the Measures Taken at the Airport for the Safe Return of Passengers
- Minister Hasan Visits Kana Hospital: LBP 750 million Dedicated for its Support and Equipment
- The Minister of Public Health Received Al-Jisser and Brought up the Mechanism of Palliative Care
- The Minister of Public Health Toured the Departments of Hotel Dieu Hospital
- Minister Hasan Announces the Conclusion of a Partnership Agreement with the Lebanese University
- The Ministry Performed PCR Tests in many Regions as Lebanon Reopens
- Minister Hasan Discussed with the French Development Agency's Director Projects to Strengthen the Lebanese Health Sector
- Minister Hasan Met with Shankiti and El-Adawi and Heard a Presentation on the Universal Health Coverage Platform
- Minister Hasan Clarifies the Grounds for the Registration of the Iranian Drug
- Minister Hasan Receives in-kind Donation from SAMS Foundation
- Minister Hasan Receives A Donation From LIA Company To Help Stop Spread of Covid-19
- Minister Hasan Discussed With Kumar the Possibility of Full Hospitalization Coverage
- The Minister of Health Met With the Unions of Pharmaceutical Manufacturers and Importers
- Assigned by President Michel Aoun, the Minister of Health Grants Dr. Walid Ammar the Gold Health Medal
- The Defense and Health Ministers Visited the Military Healthcare Center in Badaro
- The Minister of Health Met with the Order of Pharmacists
- Frem Unveils a Lebanese-Made Ventilator. Hasan: Thanks to You, We are Safe
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.694/1 and 695/1 Date 24/6/2020
- A Video Dialogue at the Ministry of Public Health: Direct Family Contact, a Major Way of Transmission
- Meeting of the National Infectious Disease Committee on 22/6/2020
- Meeting of the National Infectious Disease Committee on 15/6/2020
- In-Kind Donations from Roukoz to Bouar Hospital under the Patronage of Minister Hasan
- One billion Lebanese Pounds Allocated to Kartaba Governmental Hospital
- Minister Hasan Visits Mayfouk Hospital
- Minister Hasan Chairs a Meeting on the National Pharmacovigilance Programme
- Minister Hasan Considers Ways to Activate Food Safety Campaign with the Health Inspectors
- Meeting between Health Minister and Industry Minister: Agreement on Manufacturing Food Supplements
- Minister Hasan was Briefed on the Medical Services of Caritas and Saint Vincent Association
- Minister Hasan and his Visitors Discussed ways to Promote the Safe Tourism Investment
- Hasan Honored in Baalbeck: the Citizen Regained Confidence in Lebanon's Institutions thanks to the Ministry
- Minister Hasan Concludes his Tour in South Lebanon with a Visit to Tibnine Hospital
- Five Teams from the Ministry to Perform tests today in the Regions that witnessed a Surge in the Number of Infections
- Minister of Health Visits Marjayoun and Mays Al Jabal Hospitals
- Minister of Health From Shebaa Governmental Hospital:Caesar's Law Will Not Affect the Health System Negatively
- Minister Hasan Meets with the Vice President of the Shiite Council
- Minister Hasan Refers a Restaurant in Jemmayzeh to Public Prosecution
- Minister Hasan and the Syndicate of Laboratory Owners Agreed on the Formation of Joint Committees
- Minister Hasan Starts his Tour of Private Hospitals with a Visit to Haroun Hospital
- Minister Hasan Discussed with MP Hossein his upcoming Visit to the Islamic Council in Tripoli
- Hassan Received 13 Artificial Respirators From the Food Importers Association
- Minister Hasan Chairs a Workshop for Inspection Doctors Working in Nabatieh and South Lebanon Governorates
- Minister Hasan Meets with a Delegation of the Travel Agency Association
- Licenses of Water and Juice Companies Brought up during a Meeting between Health and Industry Ministers
- Lebanon Clinical Trials Registry (LBCTR)
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.626/1 Date 10/6/2020
- Dr. Walid Ammar Honoured by the Order of Nurses in Lebanon
- Minister of Health From Bkerki: We Hope to Handle the Files Together With the Blessing of Our Spiritual References
- Minister Hasan and Abou Sharaf Meet with the Directors of Keserwan Hospitals
- A Coordination Mechanism to be Developed between the Orders of Physicians and Pharmacists
- Minister of Health Honors DG Dr. Walid Ammar on the Occasion of His Retirement
- Minister Hasan: A Tender Will Be Launched to Purchase Medical Implants for the Ministry
- Minister of Health Honored From Baalback
- The Minister of Health Visits Barja and The Quarantine Center in Wardaniyah
- Ministers Hasan and Abdel Samad Meet with Local Authorities and UN Organizations
- The Minister of Health Hamad Hassan Visits Barja
- PCR Tests Performed on Syrians Refugees in Talhayat - Akkar
- Minister of Health: "An Expatriate Woman Transmitted The Corona Virus To 42 People In Barja and Nurseries Will Reopen"
- Médaille d’Or du Mérite National de la Santé à Walid Ammar
- Meeting of Coronavirus Committee Chaired by Minister Hasan
- Minister Hasan Discussed with MPs Ways to Support the Governmental Hospitals
- Minister Hasan Launches the Activities of the Inspection Committees in the Hospitals
- The President of the Republic, General Michel Aoun, Grants Dr. Ammar the Golden Health Medal
- Minister Hasan to NNA: The General Mobilization is Expected to be Extended for Two Weeks
- Minister Hasan and Mario Aoun Look into the Establishment of a Hospital in Damour
- PCR Tests Performed by the Ministry on Syrians in Ras al-Nabaa
- One million Masks from Sanita to the Ministry to be Distributed across the Country
- A Team from the Ministry Collects 83 Samples from the Palace of Justice, Baalbeck
- Minister Hasan Chaired a Meeting to Follow up on the Easing of Lockdown Measures
- Minister Hasan Discussed with Baalbeck Municipalities Union Development Affairs
- Minister Hasan Visits Baalbeck Community Farm
- Ministers of Industry, Public Health and Agriculture Tour Aqua la vie j'aime l'eau Factory
- Hasan Hands over Ventilators to Hermel Hospital: Thanks Iran, Kuwait and Qatar
- 355 PCR Tests Administered in Iklim Towns in the Presence of Hasan's Representative, Abdallah ana Hajjar
- Minister Hasan Toured the Ministry's Departments and Met with Heads of Syndicates
- In Honor of the Director General of Health Dr Walid Ammar
- Honoring the Director General of Health Dr Walid Ammar
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.553/1 Date 27/5/2020
- The Ministry of Public Health Honours DG Dr Walid Ammar on the Occasion of his Retirement
- PCR Tests Administered at the Justice Palace in Zahleh and the Different Governmental Hospitals
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.499/1 Date 5/5/2020
- Mufti Qablan Discussed With the Minister of Health the Measures Taken Against Corona
- Minister Hasan: Rumors About Imposing a Fine on Those Who Don't Wear Face Masks Aren't True
- At This Sensitive Stage Wearing a Face Mask is Essential For Your Safety and That of Those Around You!
- Siblin Governmental Hospital Performed 250 PCR Tests in Iklim Towns
- PCR Tests Administered to Nabatieh Fawka Residents
- Minister Hasan Tours El-Marj and Oversees the Municipality's Measures to Contain the Pandemic
- The Minister of Health from Majdal Anjar
- Hasan: There is a Real Risk and we Need everyone's Collaboration
- Memorandum Issued by Minister Hasan: COVID-19 Cases to be Announced Exclusively by the Ministry
- Minister Hasan Refers a Decision to Start Paying the Amounts due for Exceeding the Financial Ceilings
- Minister Hasan Followed Up Importing Medical Devices and Equipment Issue
- Nine Positive Cases among the Passengers Returning from Accra, Kinshasa, Frankfurt and South Sudan
- Lab Results of the Passengers Returning to Lebanon on May 3- 4
- Statement Issued by the Ministry of Public Health
- 10 Confirmed Cases Among the Passengers Returning From Lagos, and 2 Among the Expats From Paris and Pointe-Noire
- Minister Hasan Tours Rachaya and Hasbaya Hospitals
- PCR tests conducted by Teams From the Ministry in Metn District
- 108 PCR Tests Performed At Mejdlaya After One Person Was suspected to Have COVID-19
- Minister of Health Vists Deir El-Qamar Hospital and Warns Against the Risk of Community Outbreak
- Minister of Health Visits Bednayel, Kafr Dabbash, and Majdaloun: We are Still in Third Stage and Cooperation is Needed
- Minister of Health Chaired The Health Council Meeting and Stressed on the Importance of Commitment By Expatriates and Residents
- Lab Results of Passengers Returning From Moscow, Minsk, Kuwait, Douala, Bahrain, Dubai, London and Ukraine
- Medical teams of the Ministry of Public Health Have Deployed in Various Regions
- Minister Hasan Tours Jezzine Hospital: We Must Be More Careful Till Monday
- Minister Hassan visits Deir El Qamar and Jezzine Tomorrow afternoon
- Lab Results of the Passengers Returning from Nigeria and Qatar
- Lab Results of the Passengers Returning from Riyadh Six Passengers on the Flight from Qatar were Retested
- A Robot Handed out by the Lebanese University's Students to Hariri Hospital
- Hasan Received Frem and Heads of the Orders of Dentists
- Statement on the Need to Strictly Comply with Home-Quarantine and Wear Face Masks
- Minister Hasan: If COVID-19 Cases Continue to Increase, I will Seek an Approval for a 48-Hour Lockdown
- The Return of Lebanese Expatriates Committee Evaluated The Second Phase and Preparations For Third Phase
- Lab Results of Expats Returning across Masnaa and Abboudieh Border Crossings
- The Latest Lab Results for the Lebanese Expats
- Hasan: Nurseries are to be Prepared to Reopen in June
- Minister Hasan and UNICEF Representative Discussed Ways to Increase Support to Children and Students
- The Minister of Health Received From Huawei Two Technical Systems For Video Conference and AI
- Minister of Public Health and Information Minister Visited Siblin Isolation Center and the Governmental Hospital
- Minister of Health to Sputnik: We Received an Offer From Russia To Help Fight Corona
- Saturday, May 2 Flight Results
- A Team from the Ministry Carried out PCR Tests in Dhour el Shweir, Khenshara and Bekfaya in North-Metn
- The Lebanese Government Received Medical Aid from the Government of Iran
- The Minister of Public Health and the Doctors Syndicate Head Discussed Ways to Enhance the Medical Sector
- The Lab Results of the Passengers Returning from Conakry and Riyadh
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.474/1 and 475/1 Date 30/4/2020
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.462/1, 463/1 and 466/1 Date 28/4/2020
- Abdallah: The Governmental Hospitals are the First Line of Defense against Coronavirus and other Viruses
- Teams from the MoPH Performed 250 PCR Tests in Hermel
- Random PCR Samples in North Metn
- The Lab Results of the Passengers Returning to Lebanon on April 30
- Hassan to the Pharmacists: Health Security and Bill Restructuring are ahead of the Ministry's Strategy
- Lab Results of Passengers on Tuesday Flights(Second Phase of the Return of Expatriates)
- Training on the Preventive Measures at Primary Health care Centers during the COVID19 Pandemic
- Consultation Meeting between the Minister of Public Health and Representatives of Production Sectors
- World Immunization Week 2020
- Ministers Hassan and Fahmy Will Discuss Easing Mobilization Procedures
- Monitoring of COVID-19 Infection In Lebanon - 27/4/2020
- Health Minister From Rayak: We Are At An Advanced Response Stage But We Must Be Careful
- Minister Hasan: We Avoided the Bad Scenario and Going Back to Normalcy Requires Extreme Caution
- A Media Statement About Not Linking Violence to Mental Disorders
- Minister Hasan Meets with the Syndicate of the Private Hospitals Owners
- Minister Hasan Receives Beirut's MPs
- Minister Hasan and Representatives of International Organizations Agreed on a Joint Working Strategy
- Minister Hasan Follows up on the Second Phase of Random Test Examination
- Coordination Meeting between Minister Hasan and WHO Representative
- The Results of Tests Performed on 20/04/2020
- Walid Ammar à « L’OLJ » : Le Liban était préparé pour faire face à la pandémie - Nada MERHI - L'Orient-Le Jour 25 Avril 2020
- Tips to cope with stress during COVID-19
- Minister Hasan Held a Meeting to Prepare For the Second Stage of Repatriation of Expats
- Monitoring of COVID-19 Infection In Lebanon - 26/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 25/4/2020
- Launching the Second Phase of Preparing Governmental Hospitals Against Corona
- Monitoring of COVID-19 Infection In Lebanon - 24/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 23/4/2020
- Delaying Local Spread on 23/4/2020
- Minister Hasan Inspects Galilee Camp in Baalbek: We Will not Let the Pandemic Spread Inside or Outside the Camp
- Monitoring of COVID-19 Infection In Lebanon - 22/4/2020
- A Series of Meetings Held By The Minister of Health Prior to the Phase of Increasing the Number of Tests
- Hasan Visits Sir Denniye Governmental Hospital with Hawat
- Health and Telecommunications Ministers Visit Miniyeh Hospital
- Monitoring of COVID-19 Infection In Lebanon - 21/4/2020
- PCR Tests Performed at Random in Jezzine, Bint Jbeil, Baalbek and Batroun
- Delaying Local Spread on 17/4/2020
- The Minister of Public Health Discusses with the WHO Ways of Strengthening the Efforts Aimed at Fighting the Coronavirus
- Delaying Local Spread on 20/4/2020
- Minister Hasan Looks into the Measures Taken to Fight Coronavirus in Chouf
- Minister Hassan At Bahman Hospital: There Is No Financial Obstacle When It Comes To Citizen's Health
- Delaying Local Spread on 18/4/2020
- Hasan From Zahleh: The Results Today Are Good And We Are Working According to the Plan Put In Place
- Monitoring of COVID-19 Infection In Lebanon - 19/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 18/4/2020
- Additional PCR Tests To Be Performed At Random To Decide On The Next Steps
- Minister Hasan Hands Over a PCR Examination Device to Halba Governmental Hospital
- Monitoring of COVID-19 Infection In Lebanon - 15/4/2020
- Delaying Local Spread on 15/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 16/4/2020
- Delaying Local Spread on 16/4/2020
- Arrival of a Medical Aid Gift From Qatar at Rafic Hariri International Airport
- Minister Hasan Receives Chinese Gift, 3,000 PCR Examination Units and 200 Thermometers
- Delaying Local Spread on 14/4/2020
- Health Minister: No Community Spread of Coronavirus In Lebanon
- The Lab Results of the Passengers on the Planes from Paris, Jeddah and Gabon are Negative
- The Lab Results of the Passengers on the Plane from London
- Quality Assurance of Pharmaceutical Products Program: The Way forward
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.370/1 Date 27/3/2020
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.298/1 Date 5/3/2020
- Delaying Local Spread on 3/4/2020
- Minister Hassan at Saint George Hospital: We're Looking Forward With Hope to Lebanon's Bright Future
- Delaying Local Spread on 13/4/2020
- The Lab Results of the Passengers on the Planes from Kuwait, Dubai, Luanda and Rome are Negative
- Mininster Hasan Considers the Measures Taken in Jezzine against Coronavirus
- Delaying Local Spread on 8/4/2020
- Delaying Local Spread on 27/3/2020
- Delaying Local Spread on 31/3/2020
- Delaying Local Spread on 12/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 12/4/2020
- Delaying Local Spread on 31/3/2020
- The Lab Results of the Passengers on the Planes from Istanbul and Kinshasa
- Delaying Local Spread on 11/4/2020
- Monitoring of COVID-19 Infection In Lebanon - 11/4/2020
- Minister Hassan Visited Sour Governmental Hospital
- Minister Hassan Inspected Barja and Sibline Governmental Hospital
- Minister Hassan Visited Sour Governmental Hospital
- What Corona Numbers in Lebanon Actually Mean
- Delaying Local Spread on 10/4/2020
- Guidelines for the Management of Bodies of the Deceased
- Delaying Local Spread on 9/4/2020
- Minister Hasan and the Order of Engineers Discuss Ways to Coordinate Efforts against COVID-19
- Delaying Local Spread on 7/4/2020
- The Minister of Public Health Tours Bsharri
- The lab Results of the Passengers on the Planes from Madrid and Paris
- Hasan During His Visit To Saydet Zgharta University Medical Center
- Hasan During His Tour In Zgharta: We Will Work Together To Develop The Healthcare Sectors
- Minister Hasan Visits Karami And The Islamic Hospital
- Minister Hasan Concludes His Tour of North Lebanon with A Visit To Batroun Hospital
- Request for Quotation for PPE- 4/4/2020
- Request for Quotation to Purchase 70 Ventilators for the Governmental Hospitals- 28/3/2020
- Request for Quotation for PPE- 21/3/2020
- Call for Tenders
- Minister Hasan from the Airport:We Hope that there will Be no Positive Cases
- Madrid And Paris Airplanes
- List of Hospitals Eligible for SARS-CoV-2 Testing Using RT-PCR
- Minister Hasan Followed up with Representatives of International Organizations on the Refugees and Displaced Persons' Response to the Plan of the Ministry of Public Health
- The Minister of Public Health: The Isolation of some Regions has Become a Must if the Citizens Continue to Break the Rules
- Minister Hasan Followed up on the Transportation of Passengers: A Model of which we Can Be Proud
- Hasan: the Repatriation of Expats is Good Step and it was Done at a High Professional Level
- Hassan Pesented the Situation Technically
- Minister Hassan With Sahel & Bahman Hospitals
- Minister Hasan Says he Will not Hesitate to Bring to Justice the Violating Hospitals
- Delaying Local Spread on 6/4/2020
- The Lab Results of the Passengers on the Plane from Abidjan
- National Action Plan for the MHPSS Response to COVID-19
- The Lab Results of the Passengers on the Plane from Lagos
- Delaying Local Spread on 5/4/2020
- The National Mental Health Response to COVID-19
- Form to be Filled out by the Lebanese Expats
- Daily Report On Covid-19 of 5/4/2020
- Delaying Local Spread on 4/4/2020
- Delaying Local Spread
- Delaying Local Spread on 2/4/2020
- New Hotline for COVID-19
- Delaying Local Spread on 1/4/2020
- Daily Report on Covid-19 of 31/3/2020
- Issuance of the Daily Report on COVID-19 of 12/3/2020
- Daily Report on Covid-19 of 23/3/2020
- Clarification by the Ministry of Public Health
- Daily Report On Covid-19 of 27/3/2020
- Daily Report on Covid-19 of 13/3/2020
- Daily Report on Covid-19 of 14/3/2020
- Daily Report on Covid-19 of 16/3/2020
- Daily Report on Covid-19 of 19/3/2020
- Daily Report on Covid-19 of 17/3/2020
- Daily Report on Covid-19 of 18/3/2020
- Daily Report on Covid-19 of 20/3/2020
- Daily Report on Covid-19 of 21/3/2020
- Daily Report on Covid-19 of 22/3/2020
- Daily Report on Covid-19 of 25/3/2020
- Daily Report on Covid-19 of of 24/3/2020
- Daily Report on Covid-19 of 26/3/2020
- Daily Report on COVID-19 of 28/3/2020
- Daily Report on Covid-19 of 15/3/2020
- Daily Report on COVID-19 of 30/3/2020
- Daily Report on Covid-19 of 29/3/2020
- Minister Hasan Confirms That Ten Hospitals Are Now Ready to Take Part In the Fight Against the Corona Virus
- Issuance of a Circular and Four Administrative Memorandums Related to COVID-19
- LSIDCM Guidelines for the Management of COVID19
- An Informative Video Where the Minister of Public Health Dr. Hamad Hassan and the Minister of Information Dr. Manal Abdel Samad Participated
- Daily Report On Covid-19
- Awareness Campaign on Thalassemia Prevention
- Minister Hasan Discussed with a Palestinian Delegation Measures to Ensure the Protection of the Camps and Received a Number of Researchers
- Minister Hasan Toured Al-Bouar Hospital: We have Entered the Second Phase of Equipping the Governmental Hospitals in all Districts and Governorates
- Statement Issued By Notre Dame de Secours-Jbeil Hospital
- Minister Hassan Meets with Minister Ohanian
- Minister Hasan Presented to the Health Committee the National Plan and Revealed the Problems That Hindered the Implementation of the World Bank Loan
- Hasan Chaired the Meeting of the National Committee For Transitional Diseases and Discussed Signing A Contract With Private Laboratories To Conduct Laboratory Tests Free of Charge
- When Should We Do A Corona Test? And Where?
- Warning Regarding Hydroxychloroquine Drug
- Are we Ready for the Outbreak of the Epidemic Locally? Minister of Public Health Dr. Hamad Hassan Explains the Readiness of the Health Sector in Lebanon to Respond to the Corona Virus
- New Website Launched by the Ministry of Information Regarding Coronavirus Latest News in Lebanon
- Issuance of Decision of the Minister No. 359 of 20/3/2020 on How to Deal with Coronavirus Patients who are Showing no or mild Symptoms and those who made Recovery while still Tested Positive
- Minister Hasan's Statement Denies the Current News About the Existence of A Decision to Isolate Some Areas of Lebanon
- COVID-19 Testing Procedure Discussed during a Meeting between the Minister of Public Health and the Syndicate of Laboratory Owners
- Daily Report on Covid-19
- Daily Report on Covid-19
- Statement Issued on March 16, 2020
- Clarification From Rafik Hariri University Hospital on Details of Death in Corona Emergency
- COVID-19 Confirmed Cases by Casa, Lebanon,21 Feb-16 March 2020
- Coronavirus Disease 2019 (COVID-2019) National Health Strategic Preparedness and Response Plan
- The Daily Report on the Latest COVID-19 Updates at Rafik Hariri University Hospital
- Minister Hasan: Two Patients have Recovered from Coronavirus and a Solution for Hariri Hospital Workers has been Reached with the Premier's Support
- Issuance of Memorandum No. 53 of 17/3/2020 on filling out the traveller's form on board all the planes flying to Lebanon
- Memorandum No. 53 of 17/3/2020 on filling out the traveller's form on board all the planes flying to Lebanon
- Issuance of Circular No. 52 of 16/3/2020 on Reporting the Results of COVID-19 Tests
- Minister Hasan Urges the Transport Sector to Abide by the State of General Mobilization
- Minister Hasan’s Press Conference in Rafik Hariri International Airport With the Chinese Ambassador
- Issuance of New Minister Resolutions Regarding New Measures In Response to the Corona Epidemic
- Press Release 13-3-2020
- Press Release
- Minister Hasan Chaired a Coordination Meeting to Equip Governmental Hospitals to Receive Corona-Infected Patients
- Minister Hasan: Eight Governmental Hospitals are now Equipped to Increase the Carrying Capacity
- Minister Hasan Discussed With UNICEF Representative the Strengthening of Cooperation Programs
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- Minister Hasan to Hold a Meeting With the Parliament's Health Committee in the Afternoon
- Minister Hasan's Diplomatic Activity
- Statement Issued on March 11, 2020
- The First Fully Recovered Case From Coronavirus
- Guidance for Self-Isolation at Home
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- Issuance of the Daily Report on COVID-19 of 11/3/2020
- Joint News Conference between Minister Hasan, WHO and UNICEF on Coronavirus Control
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- Press Release on the Issuance of COVID-19 Laboratory Test Results
- Press Release on the Issuance of the Medical Reports during the COVID-19 Global Health Emergency
- Issuance of Memorandum No. 48 of 10/3/2020 by the Minister on the Laboratory Diagnosis of Coronavirus Cases
- Minister Hasan Considers With the International Organizations Ways to Develop Cooperation Programs
- The First Coronavirus Death Confirmed in Lebanon
- MoPH Launches a New Awareness Campaign on COVID-19
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- Ways to Respond to Coronavirus Crisis Discussed in a Meeting between Minister Hasan and a World Bank Delegation
- Issuance of Circular No. 46 of 9/3/2020 by the Director General Concerning the Measures that Should be Taken by the Health Institutions to Prevent the Spread of Coronavirus
- Statement Regarding Laboratory Analysis of Coronavirus Suspected Cases
- Minister's Decision on the Closure of Nurseries Till March 15
- Issuance of the National Epidemiological Surveillance Program Bulletin on COVID-19 on 8/3/2020
- The Daily Report on the Latest COVID-19 Updates at Rafik Hariri University Hospital
- Rafik Hariri University Hospital Report: The Total Number of Infections in Lebanon Increased to 16
- Minister Hasan's Visit to Bouar Hospital
- Minister Hasan's Tour in Akkar and Tripoli
- Statement Issued on March 4, 2020 Regarding nCoV-19 Laboratory Tests Done In Private Laboratories
- Coverage of Minister Hasan's Visit to Bouar Hospital At Noon
- Statement of 6/3/2020 on the coronavirus case at Notre Dame de Secours Hospital
- A New Confirmed Coronavirus Case In Lebanon
- Minister Hasan Holds a Meeting to Agree on a Cooperation Strategy between the Hospitals
- Report of Rafik Hariri University Hospital: Coronavirus Cases Increased to 15
- Definition of Suspected COVID-19 Case
- Memorandom No. 44 of 5/3/2020 Issued by the Minister on Avoiding Travelling and Crowded Places to Prevent the Outbreak of Coronavirus
- Coordination Meeting on Coronavirus Control between Minister Hasan and Representatives of International Organizations
- Al Jadeed TV Report on the Preventive Measures at the Ministry of Public Health
- COVID-19- Daily Situation Report
- COVID-19- Daily Situation Report
- COVID-19- Daily Situation Report
- New Press Release Issued on 3/3/2020
- Agence France-Presse Report on the Ministry of Public Health
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- Media Tour of the New Isolated Section for Coronavirus Patients at Rafik Hariri University Hospital
- Press Conference for the Minister of Public Health Tomorrow
- Issuance of the Circular No.38 of 2/3/2020 to the Primary Healthcare centers on the need to abide by the preventive measures against COVID-19
- Rafik Hariri University Hospital: The News Saying that a Staff Member of the Hospital was Quarantined is Completely False
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- Three New Cases of Coronavirus Confirmed
- Statement of March 2, 2020 on the Preventive Measures Against COVID-19 in the Institutions That Have Contact With the Public
- The Ministry of Public Health Confirms That the Epidemiological Situation in Lebanon is Still in the Phase of Containment
- The Ministry of Public Health Warns against the Spread of Fake News
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- The Ministry of Public Health: Three New Cases of Coronavirus Confirmed
- Rafik Hariri Hospital: 3 New Cases Confirmed and 16 Quarantined
- COVID-19 Outbreak Level in Lebanon Compared to Other Countries
- Statement of Clarification Issued by the Press Office
- Decision on the Closure of Nurseries
- Minister Hasan Postponed His Visit to North-Lebanon Hospitals
- The Ministry of Public Health Reminds the Decision to Close the Nurseries till March 8
- The Daily Report on the Latest COVID-19 updates at Rafik Hariri University Hospital
- Three New Cases of Coronavirus Confirmed
- COVID-19- Daily Situation Report
- Press Release Concerning Coronavirus Situation in Lebanon
- Statement Issued by the Ministry of Public Health
- Issuance of the Circular of the Minister No.36 of 27/2/2020 on the Preventive Measures against Coronavirus in Nurseries
- Hasan Visited al Mahdi High School in Baalbeck: the Situation is under Control and there is no Need to Close the Schools
- Hasan Toured Baalbeck Governmental Hospital
- The Ministry of Public Health: Third Case of Coronavirus Confirmed
- Countries Requiring Yellow Fever Vaccination for Incoming Travelers
- Details of the Meeting With Dr. Walid Ammar Regarding the MoPH Measures to Limit the Spread of Coronavirus
- National Health Accounts 2017
- Drugs National Guidelines
- National Health Accounts 2016
- Minister Hasan Announces First Coronavirus Case in Lebanon
- Minister Hasan and the Chinese Ambassador Followed up on the Developments Regarding the Control of Coronavirus Spread
- Statement Issued by the Ministry of Public Health
- Hasan Received the Ambassador of India and the Chargé d'affaires of Iraq
- Hasan and Hoballah Seek to Promote Bilateral Cooperation in Pharmaceutical Industry and Food Safety
- MoPH-MEHE Joint Initiative for Cooperation with the Medical Students on Measures against the Coronavirus
- Memberships in International Organisations
- Dr Walid Ammar Officer in the French National Order of Merit
- La Remise des Insignes d'Officier dans l'Ordre de la Couronne de Belgique au Docteur Walid Ammar
- Award of the Dr A.T. Shousha Foundation Prize and Fellowship To Dr. Walid Ammar
- Provision of TPA Services in Primary Healthcare Centers (Invitation of Expression of Interest EOI for Specialised Companies)
- Rafik Hariri Hospital's Latest Updates on Coronavirus: 32 People have been Tested for Coronavirus; 7 of them Needed to Enter Quarantine
- Guidance on Home Isolation
- Issuance of Minister Decision No. 2648/1 and Administrative Memos 132 and 133 of 24/12/2019 on the Implementation of the Barcode System on Imported Drugs
- Press Release about the Launching of the Maternal Mortality National Report- A Success Story in Lebanon
- Launching Event
- President Aoun Welcomed the Minister of Public Health and the Former Deputy Sukariya
- Health System Resilience in Lebanon: A Consistent Progress amidst Political Instability- June 2019
- The Minister of Public Health Discussed With Al-Khatib the Protective Measures Against Coronavirus
- Rafik Hariri Hospital's Latest Updates on Coronavirus: 25 People have been Tested for Coronavirus; none of them Needed Hospital Care
- Details of the Press Conference Held by Minister Hasan at Rafik Hariri Hospital
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.207/1 Date 20/2/2020
- Meeting Chaired by Dr. Walid Ammar to Discuss the Difficulties in the Implementation of the Code of Ethics for Medicinal Products Promotion
- Minister Hasan Meets with a Delegation of Baalbek Municipality
- The Presidency of the Central Inspection Commends the Performance of the Minister of Public Health Dr. Hamad Hasan
- Statement Issued by the Ministry of Public Health
- The Ministry of Public Health and the Lebanese Pediatric Society urge parents to get their Children Vaccinated against Measles
- Hasan Visited the PHC center in Aarsal
- The Ministry of Public Health Reminds the Pharmacies to Adhere to the New Prices of Infant Formula
- Influenza Surveillance Bulletin 15 February 2020
- Statement Issued by the Ministry of Public Health on the Measures Followed with Regard to the People Coming from China
- The International Day for Childhood Cancer 2020
- Meeting between Minister Hasan and the Syndicate of Private Hospitals
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.172/1 Date 12/2/2020
- Hasan Calls on to Seek Information on Coronavirus from the Competent Authorities at the MoPH
- Statistical Bulletins
- Minister Hassan was Briefed on Precautions to Prevent Corona Transmission at Rafic Hariri International Airport
- Issuance of Infant Formulas (from 0 to 1 year) Public Price list
- H1N1 a Seasonal Virus: The Moph Issues a List of Precautionary Steps
- Minister Hasan Visits Health Centers in Baalbek
- Circular Issued by the Minister of Public Health on Hospitalization
- Memorandum No.16 of 7/2/2020 Issued by the Director General on the Request of Information from the Pharmaceutical Institutions
- Influenza and Coronavirus Prevention Guidance
- Statement Concerning The Ship Coming From The Far East
- No Cases of Coronavirus Infection among the Lebanese in Wuhan
- Minister Jabak Receives the Leadership Award in Healthcare
- The Decision on the Reduction of Infant Milk Prices to Enter into Effect next Week
- Prevention Guidance On World Cancer Day
- Statement Concerning The Ship Coming From The Far East
- Statistical Bulletin 2018
- Meeting between the Minister of Public Health and the Lebanese Order of Physicians
- The Ministry of Public Health Reaffirms that there are NO Coronavirus Cases in Lebanon
- Statement Issued by the MoPH on the nCov-2019 in Lebanon
- The Health Situation on Board the Ship Coming from the Far East to Lebanon
- Infant Milk at Lower Prices as agreed with the Central Bank
- Workshop this Monday at the MoPH: Guiding Principles for Media Specialists
- Minister Hasan Met with a Delegation from the World Bank and the Inspection Doctors and Reiterates the Absence of any Case of Coronavirus in Lebanon
- Internal Tour of the Minister of Public Health and Disciplinary Measures against the Employees who were Absent without Justification
- Statement Denying Allegations of the Emergence of the First Case of Corona Virus Infection in Tripoli
- Unexpected Visit of the Minister of Public Health to the Airport
- Influenza Surveillance Bulletin 25 January 2020
- Minister Hasan after Meeting with the Chinese Ambassador: No Cases of Coronavirus-Infected Lebanese in China
- Influenza and Prevention
- Influenza Virus
- Minister Hasan: There is no Need to Panic about Influenza
- MoPH: Influenza Epidemiological Indicators within the Expected Level
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.143/1 Date 21/1/2020
- Clarification about the Health Coverage of Road Traffic Accidents
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1927/1 Date 19/9/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1912/1 Date 18/9/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1944/1 Date 24/9/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 2245/1 Date 30/10/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No. 2305/1 Date 12/11/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2462/1 Date 02/12/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2586/1 Date 18/12/2019
- Handover Ceremony at the Ministry of Public Health
- The Arab Hospitals Federation: It is an Honour to Grant Minister Jabak the Leadership Award in Healthcare
- Jabak: Salameh Denounced the Agreement
- Jabak: a Temporary and Partial Solution for the Provision of Medical Supplies is Reached
- Dr Jabak was Briefed on the Private Hospitals' Problems and the Difficulty of Securing Medical Supplies
- Feeding Infants and Young Children in Exceptional and Difficult Circumstances
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.3/1 and 5/1 Date 3/1/2020
- Statement Issued by the Media Office: All Allegations and Claims are Referred to the lebanese Justice
- Jabak: There will be no Shortage of Cancer and Chronic Disease Medicines for the First Month of the Year
- Statement of the Minister of Public Health's Office
- Statement of the Minister of Public Health's Office
- Ministry of Health Regarding Influenza: Epidemiological Indicators Are Still Within the Nationally Expected Levels
- Issuance of Decision No. 2605/1 Date 19/12/2019 Regarding the Continuation of the Implementation of Decision No. 1/744 until the Completion of the Implementation of the First Article and Giving Priority to Registration for Generic and Biosimilars Drugs
- Holiday Gathering Held by Minister Jabak at the MoPH
- Minister Jabak was Briefed on the Problems Encountered By the Nursing Sector and Promised To Follow Up on Cuts in Salaries
- Related Articles
- Jabak Held Meetings on the Import of Narcotics and Medical Supplies and Equipment, Noting the Growing Concerns of the Lebanese Citizen
- Jabak participated in Doha Forum and met with Sheikh Abdullah Bin Mohammed
- Issuance of the Minister's Decision No. 2548/1 of 11/12/2019 on the Adoption of Infant Formula Pricing
- Issuance of the Minister's Decision No. 2548/1 of 11/12/2019 on the Adoption of Infant Formula Pricing
- Jabak Arrives in Qatar to Participate in Doha Forum
- Jabak Addressing the Conference in Oman: The Lebanese Health Care Sector has Achieved progress in attaining the SDG target on NCDs
- Launching of Polio and Measles Vaccination Campaign in Akkar
- Launching of Polio and Measles Vaccination Campaign in Akkar
- Jabak's visit to Oman began with the global meeting of the Arab Health Ministers
- Jabak heads to Oman to take part in the meeting of the World Health Organization
- Launching of the National Measles Vaccination Campaign
- Jabak Discussed with the Ambassador of Egypt Ways to Promote Bilateral Cooperation in the Field of Health
- Jabak: We have Abolished Monopolies on Medicines and Prices will be Reduced by Nearly One Third
- Jabak Inaugurated Ghobeiry Medical Center: We Seek to Rehabilitate the Governmental Hospitals
- Jabak: Banque du Liban Pledged to Provide Medical Supplies
- Don't let your Life end in Silence Call the Lifeline 1564
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.2411/1 and 2412/1 and 2413/1 Date 25/11/2019
- Office of the Minister of Public Health: The Pharmaceutical Storage Project Raised the Medicine's Quality to Higher Levels
- World Antibiotic Awareness Week 2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.2345/1 and 2346/1 Date 18/11/2019
- Jabak's Media Office: A Young Child from Tripoli to Receive Medical Care at the Expense of the Ministry of Public Health
- Assessment of the Quality of Services at the Primary Health Care Centers
- National Immunization Strategy 2017-2022
- EPI Strategy and Multi Year Plan
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.2265/1 , 2267/1 and 2268/1 Date 6/11/2019
- Issuance of Decision No. 2291/1 of 7/11/2019 on Printing the Expiration Date on Drugs' Packaging
- Statement of the Minister of Public Health's Office in Response to the Allegations and False Claims Regarding the Patient Ramadan
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.2153/1 and 2162/1 Date 29/10/2019
- Emergency Primary Health Care Restoration Project towards Universal Health Coverage in Collaboration with World Bank
- Jabak Instructed all Hospitals to Admit the People Injured in the Fires at the Ministry's Expense
- Jabak in Iran to Participate in the Regional WHO Conference
- Jabak Heads to Iran to Attend the Regional WHO Conference
- Jabak Tours Health Centers in Chouf
- National Breast Cancer Awareness Campaign 2019
- Jabak Launched the Largest National Breast Cancer Awareness Campaign
- Maneuver in Kfar Falous Attended by more than 932 Medical Professionals Jabak: the First of its Kind in Lebanon
- Jabak Declared the Ministry of Public Health a Smoke-Free Building and Outlined Steps to Implement Law No.174
- Activities and Events
- Jabak Sponsors a Charity Dinner in Support of Cancer Patients at Makassed Hospital
- Jabak Launched the National Awareness Campaign for Cardiovascular Risks in Diabetes Patients
- Jabak Inaugurates a Primary Healthcare Center in Dhour Choueir
- Jabak Inaugurates a Radiology Center in Bhannes
- Jabak Opened the 11th International Congress of Neurology
- Jabak Represented President Aoun at "Children Cancer Center" Dinner: We Decided to Support the Center
- List of Essential Medicines Lebanon 2018
- Launching of the First National Conference on Person-Centered Care at Bellevue Medical Center under the Patronage of the Minister of Public Health
- The Minister of Public Health Represented President Aoun at the Awareness Campaign on Sudden Cardiac Arrest
- The Ministry of Public Health Launched the National Initiative for Mental Health in the Workplace
- Mental Health Awareness Campaign 2019
- Jabak Discussed with Jamali Tripoli's Health Projects and Received the Swiss Ambassador and the UNDP Director
- Jabak Toured Arwan Pharmaceutical Industries in Jadra
- National Mental Health Awareness Campaign 2019
- Jabak: Baalbek-Hermel Governmental Hospitals have been Put on the Map of Development
- Jabak Inaugurated a Pharmacy for Chronic Disease Medicines and a Neonatal Unit at Hermel Governmental Hospital
- Jabak Opened a Pharmacy for Chronic Disease Medicines at Baalbek Governmental Hospital
- Jabak Represented President Michel Aoun at the Conference of the Lebanese Fertility Society
- The Minister of Public Health Reveals the Circumstances behind the Case of Mohamad Rima and Launches the National Asthma Campaign
- Issuance of Decision No. 1894/1 of 17/09/2019 on the Necessary Preparations for the Implementation of the 2D Barcode on Drugs
- Jabak Opens the Regional Meeting with the World Health Organization on Strengthening Pharmacovigilance Systems
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1859/1 Date 12/9/2019
- Jabak: Al-Fanar Hospital will be Reopened and the Works nearby are Carried out in a Private Land and are not Related to the Hospital
- Minister Jabak Takes Part in the Global Vaccination Summit in Brussels
- jabak from nabatieh
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1807/1 , 1815/1 and 1819/1 Date 4/9/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.1666/1 , 1667/1 and 1669/1 Date 21/8/2019
- Jabak Opened the Heart Failure Conference at Hotel Dieu de France Hospital
- Jabak Opened the AUBMC Theranostics Conference
- Training of Trainers on Hospital Death Certification
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1638/1 Date 19/8/2019
- Minister Jabak Launched the National Awareness Campaign on Migraine
- Jabak Discussed with his Belarusian Counterpart Ways to Develop Cooperation in the Field of Medicines and Medical Equipment
- Jabak Meets al-Alwan at the Start of his Visit to Beirut
- Meeting Chaired by DG Dr. Walid Ammar with the Health Syndicates to Discuss the next Phase of the Implementation Plan of the Drugs Barcode Project
- Hariri was Briefed by al-Alwan and Jabak on the items of the memorandum of Understanding Signed by Lebanon and Iraq
- The International Day for the Prevention of Over Dose
- President Aoun Meets with the Lebanese and Iraqi Ministers of Health
- Tour by Ministers Jabak and al-Alwan to Three Hospitals
- Results of Laboratory Technician Competence Exam for Students Applying for Professional Practice License of 10 and 11 July 2019
- Documentary on Poliovirus and Acute Flaccid Paralysis Surveillance in Lebanon
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1700/1 Date 23/8/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1682/1 Date 22/8/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1531/1 Date 2/8/2019
- "Have You Heard about 47?" Campaign
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1606/1 Date 9/8/2019
- Jabak Received Delegations from Akkar and North Lebanon
- Jabak Discussed with Delegations from Akkar the Situation of the Region as to the Hospitalization, Medicine and Pollution
- Jabak: Infants shall Have the Right to Breast Milk that Contributes to their Health and Immunity
- Jabak Holds a Joint Press Conference with the Syndicate of Hospitals and the Order of Physicians
- Drugs Public Price List according to the exchange rate No. 19/2/31119 issued on 30/7/2019 based on Minister's Decision No. 1558/1 issued on 2/8/2019 and published in the official gazette on 8/8/2019
- Second Training Session of Proficiency Testing in Microbiological Laboratories in Active Hospitals in Lebanon
- Launching of the National Awareness Campaign on Obesity 2019
- Jabak Launched the National Awareness Campaign on Obesity
- Jabak Inaugurates the American Diagnostic Center; the first MoPH-Contracted Laboratory and Radiology Center
- The Moph Denies Claims over the Establishment of a New Governmental Hospital in Baalbeck Funded by Iran
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1430/1 Date 24/7/2019
- Brigadier Hamdan Meets Minister Jabak: A Breakthrough in Health Security will be Achieved
- The Ministry of Public Health Explains the Circumstances of Hepatitis A in Sarafand
- Jabak and the International Red Cross Launched a Project to Standardize the Prosthetic and Orthotic Services
- Minister of Public Health Chairs a Preparatory Meeting for Beirut Forum of Arab Hospital Federation
- Celebration of Doctors without Borders' One-Year Anniversary of Running the Maternity Center at Rafik Hariri University Hospital under the Patronage of Minister Jabak
- Jabak Toured Nabatieh and Visited Raad and Sadek: Austerity Measures do not Apply to Health Care and South Hospitals are not Rejecting any Patient
- Jabak: the Statistics of the Ministry are Monitoring the Spread of Drugs in Schools and Universities
- Jabak at the Opening of a Cardiac Catheterization Department at Al Mortada Hospital, Baalbek: We are not among those who Compromise the Health of the Citizen and the Country
- Minister Jabak Presided over a Coordination Meeting at the Ministry before Heading to Iraq
- Jabak and El Hassan Launched Stop the Bleeding Training Program
- PSO Projects
- Jabak Signed with his Iraqi Counterpart a Memorandum of Understanding that Recognizes the Quality of the Lebanese Drug and Meets the Iraqi's Needs
- Jabak Meets Iraq's Prime Minister and Interior Minister during his Tour
- Jabak Signed a Memorandum of Understanding with the Red Cross Concerning the Prosthetics and Orthotics
- Jabak Introduced Ways to Cut Drug Prices and Confirmed Raising the Financial Ceiling of Al Rassi Governmental Hospital to LL 6 billion
- Statement on the Demands and Overdue Payments of the Governmental Hospitals' Employees
- Jabak: We are Establishing a New Governmental Hospital in Baalbek and Improving the Level of the Governmental Hospitals in the Governorate
- Statement Concerning the Disagreement between Saida Governmental Hospital's Director and Employees
- ESPISP II
- PHC Activities
- Vital Data Observatory
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1222/1 Date 1/7/2019
- High-level meeting on the mental health reform in Lebanon- midterm evaluation results and priority-setting
- Improving mental health care in humanitarian crises
- Improving mental health care in humanitarian crises
- National Awareness Campaigns
- Le Ministère de la Santé Publique au Liban Perd un Grand Ami
- Minister Jabak Representing President Michel Aoun at the IMS Conference
- Jabak Launched the Continuous Pharmacy Education Program in Collaboration with the Order of Pharmacists
- Jabak Visiting Rayak Hospital: any File Smacking of Corruption will Result in the Prosecution of the Hospital and the Termination of its Contract with the MoPH
- Jabak Confirms during the Health Committee Conference the Pharmaceutical Sector's Need for Accountability
- Jabak Touring West Beqaa Hospital Sohmor: the Price of Drugs for Incurable Diseases will be Significantly Reduced
- National Mental Health Awareness Campaign 2015
- Improving humanitarian crisis response policy and practice: mental health and psychosocial support coordination in Lebanon
- Gallery
- Jabak Launched the National Awareness Campaign on High Blood Pressure
- A Second Meeting between Jabak and the Red Cross Head of Delegation to Promote Cooperation in Common Areas of Work
- Jabak Discussed with Audi Topics Related to the Hospitalization and Health Sector
- Decision of the Minister of Public Health: Banning of any Food Supplement Advertisement in the Mass Media
- Jabak Inspects Benta Industries
- Jabak Tours Pharmaline Manufacturing Company: We have to Further Support the Pharmaceutical Factories
- Jabak at the Luncheon Held by the Syndicate of Pharmaceutical Industries
- Jabak Inspects Algorithm's Facilities in Zikrit as part of his Tour of Pharmaceutical Factories
- The Representative of Jabak at the Opening of a Health Conference in Sidon
- Jabak at the Opening of a Mother and Child Care Center in Douris
- The Owners and Workers of Private Hospitals Staged a Sit-in before the MOPH's Premises
- Hasan Met with Jabak: Regional Health Care Centers and Hospitals Need to be Supported
- text
- National Awareness Campaign on the Reproductive Health 2018
- National Campaign for Prevention of Cervical Cancer 2017
- Statement of the Minister of Public Health on al-Aridi's Case
- Statistical Bulletin 2016
- Jabak in Bkerki: The Austerity Measures will not Affect the Ministry of Public Health
- Jabak at Dar El Fatwa: Consensus in Lebanon is a must
- Statistical Bulletin 2017
- F-Diseases’ Surveillance Data
- D-Epidemiology
- Jabak Received a Delegation of Muslim Scholars Gathering
- Launching of the National Awareness Campaign on the Reproductive Health
- National Awareness Campaign on Child Immunization 2018
- Jabak Opened the Lebanese Society of Gastroenterology's Conference
- Hasbani Launched the National Awareness Campaign on Child Immunization
- President Aoun Discussed with the Minister of Public Health the Situation of the Ministry
- Jabak Received an Invitation from the Democratic Gathering to Visit Chouf
- Hasbani Launched with "Aa Stouh Beirut" Association the National Campaign for Prevention of Cervical Cancer: We will Continue to Raise Awareness to Fight Diseases and Pain and Reduce the Medical Bill
- Stories From the Field
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1046/1 Date 11/6/2019
- Jabak Follows up with the World Bank the Launching of the Soft Loan Project for the Health Care System
- Jabak on Pharmacist's Day: a Strategic Decision to Establish a Central Lab
- Jabak Launched the No-Tobacco Campaign from Hotel Dieu Hospital
- Jabak Launched the No-Tobacco National Strategy
- Jabak Received the UNICEF Regional Director and Discussed with Alame the Introduction of the AED Device
- Training of MoPH Staff on CPR and AED
- Reproductive Health Services
- Invitation to Attend the Launching Ceremony of the National Tobacco Control Strategy
- Health Facility Locator
- Press Conference on the Outcomes of Minister's Jabak International Meetings in Geneva
- Food Safety
- Medicines Available Free of Charge in MOPH
- Public Hospitals News
- Jabak Visits Dahr El Bachek Governmental Hospital: Austerity Measures Can Affect all the Ministries, Except for the Ministry of Public Health
- Jabak Tours Baabda Governmental University Hospital
- Jabak Tours Zahrani and Tyre: The Economic Situation is Difficult. Austerity Measures to be Applied to everything, Except for Health Care Sector
- Jabak Touring Dinnieh: We will Launch next Week a Tender for Equipping Governmental Hospitals as Befits the Lebanese Citizen
- Jabak Visits Hasbaya and Rashaya Governmental Hospitals
- Jabak from Ehden Governmental Hospital: We will Find a Way to Support the Employees and Secure an Amount for the Hospital to Continue to Operate
- Jabak Visits Bechareh Governmental Hospital
- Jabak Toured Rafik Hariri University Hospital and Confirmed his Commitment to Fully Support it
- Jabak Toured West Bekaa Hospitals: I Apologize on behalf of the Lebanese State for Failing to Fulfill its Responsibilities towards the Region's Residents
- Jabak Toured Elias Hrawi Governmental Hospital: The Hospital Lacks some Equipment and we will Provide it
- Jabak Visited the Mais al-Jabal, Tebnine and Bint Jbeil Hospitals: I will Try to Support the Disadvantaged Areas with the Possible Means
- Jabak Visited the Mais al-Jabal Governmental Hospital
- Minister Jabak Toured El Hermel's Hospitals and Promised to Secure the Necessary Equipment
- Jabak from Halba Hospital: We will Increase its Budget to LL 7 billion and we won't Let any Hospital Deny a Patient's Admission
- Jabak Toured Nabih Berri Hospital and Praised its Equipment. We will Cancel Contracts with Hospitals that Refuse Emergency Patients
- Minister Jabak Delivered Lebanon's Statement at the 72nd Session of the World Health Assembly
- Directory
- Laws Violation
- HACCP Certificates
- Nominations
- Minister Jabak's Second Day in Geneva; Bilateral Meetings Held and Lebanon's Statement to be Delivered in the afternoon
- Jabak Stressed that Transparency and Public Trust Helped Overcome the International Concerns
- Jabak's off to Geneva to Attend the WHO's Assembly
- Jabak Launched Hemophilia Awareness Campaign and Listed the most Important Factors for the MoPH's Promotion
- Regulation of research
- Jabak and Abou Faour Agreed on Procedures to Protect the Pharmaceutical Industry
- Research
- Mapping of services for response to substance use disorders report- 2017
- Needs of women with substance use disorders in Lebanon - 2019
- Accreditation standards for residential substance use rehabilitation programmes - 2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.822/1 Date 14/5/2019
- Minister of Public Health Receives Okais and Wahhab
- Statement Issued by the Media Office of the Minister of Public Health Dr. Jamil Jabak
- Minister of Public Health Meets with the Scientific Committee of the Arab Healthcare Industry Forum
- Practical Guide for Media Professionals on the Coverage of Mental Health and Substance Use
- Jabak Launched the National Heart Failure Awareness Campaign
- Minister of Public Health Meets with a Delegation of the World Bank and the Ambassador of China
- Minutes of meetings
- Jabak Chaired a Meeting with the WHO and Received the Ambassadors of the Sultanate of Oman and Sri Lanka
- Minister Jabak Met with Heads of Syndicates in the Health Sector to Discuss the Overdue Payments to Hospitals and Doctors
- High-level meeting on the mental health reform in Lebanon- midterm evaluation results and priority-setting
- Statement on the Latest Developments in the Case of Patient Diana Akel
- Minister of Public Health Launched the National Colon Cancer Awareness Campaign
- Jabak Launched Diabetes Awareness Campaign for a Safe Fasting during Ramadan
- Statement Concerning the Death of Raghed Kais
- Jabak Discussed with MP Sami Fatfat the Health Needs in Northern Lebanon
- Press Release on the Occasion of World TB Day
- Jabak Meets with the Association of Child with Kidney Disease
- NCR tables - Pediatric cases
- The Office of the Minister of Public Health: The Patient Diana Akel is Covered by the NSSF, but Minister Jabak Exceptionally Requested to be Provided with the Necessary Treatment at the Expense of the Ministry
- Jabak Visiting Tripoli: the Situation is Difficult in Northern Lebanon and I am Seeking to Raise the Financial Ceilings for the Private Hospitals Despite Austerity
- On World Autism Awareness Day, Conference and Painting Exhibition at the MoPH
- Jabak and the Ambassador of Cuba Looked into Ways of Collaboration in the Pharmaceutical Field
- Jabak Announced the Construction of a New Governmental Hospital in Arsal
- Jabak Starts his Tour in Beqaa with Maqne Health Care Center
- National Breast Cancer Awareness Campaign 2017
- Jabak Toured Karantina Warehouse for Drugs and Received a Grant from the Ambassador of Brazil
- Jabak Considers Ways to Open the Turkish Hospital that Remains Closed in Sidon
- Jabak Visits "Al Bouar" Governmental Hospital and Primary Health Care Center
- Jabak Assured the Governmental Hospitals Employees that he would Change the Boards of Directors that Fail to Fulfill their Tasks
- Ministry of Public Health Efforts to Promote Palliative Care Services
- Practical Launching of the Proficiency Testing at Microbiology Labs in Private and Public Hospitals
- Jabak Meets Members of the Lebanese Community and Reaffirms his Commitment to Upgrade Services at the National Level
- Jabak Addresses the Health Care Conference in Kuwait
- Jabak Arrives in Kuwait and is Set to Meet the Lebanese Community this Evening at the Embassy
- Minister of Public Health's Office: 4 People were Bitten by Snakes within two Days and the Reports on the Case of one of them are Exaggerated
- Jabak off to Kuwait to Take Part in the Arab Health Care Development Conference
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.592/1 Date 8/4/2019
- Jabak: The Civil Service Board's Role must be Activated and Examinations should be Conducted for any Position in the Hospitals' Administration
- Jabak Received the Iranian Health Attaché
- The Media Office of the Minister of Public Health Explains the Cause of Death of Melania Hajj and Marvin Hobeiqa
- The Ministry of Public Health Denounces the Policeman's Attack against a Woman with Mental Disorder
- Jabak Represents President Aoun at the Ninth Arab pharmaceutical and Healthcare Industry Business Development Forum
- President Aoun and Minister of Public Health Discussed the Situation of the Health Sector
- Jabak Tours Al-Rasoul Al-Azam Hospital
- Jabak Received Girard and Representatives of Baalbeck-Hermel Bloc
- Jabak and the Ambassadors of China and Qatar Discuss Ways of Strenthening Health Cooperation
- Press Release on a Malaria Case
- Minister of Public Health Suspends the Contract with N.D. Maritime Hospital Jbeil Following the Initial Investigation into the Death of the Child on Friday Evening
- Jabak Received a Delegation of Akkar Figures
- Jabak Participating in the Jubilee Ceremony of the Islamic Hospital
- Jabak Inspects the Islamic Hospital with Karameh
- Jabak Completing his Tour in Tripoli
- Jabak Visits the City University and Al-Karameh Institutions in Tripoli
- Arbid Representing Jabak at the Conference on Vascular Surgery
- Back from Turkey, the Child Othman Received by the Representative of Jabak, Ayad
- Jabak Received the Red Cross Head of Delegation, the Swiss Ambassador and a Delegation of School Students
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.525/1 Date 28/3/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.515/1 Date 27/3/2019
- Jabak Meets with a Delegation of the Arab Hospitals Federation
- Jabak Launched the Annual Kidney Diseases Prevention Campaign
- Jabak Launched the Awareness Campaign on Sudden Cardiac Arrest in Young People
- Jabak Submits Forms to the Governmental Hospitals to Fill out
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.495/1 Date 26/3/2019
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.493/1 Date 26/3/2019
- Jabak Visited Marjayoun Hospital to Improve the Health Services and Conditions of the Governmental Hospitals in Disadvantaged Areas
- Minister Jabak Meets with the Administrative Officials of 90 PHC Centers
- Jabak from Bnachii: the Ministry of Public Health is not a Party Ministry and any Sanction in it will Leave Impacts on all the Lebanese People
- Jabak from Saydet Zgharta University Medical Center: It Gladdens my Heart to see a Hospital of a Similar Level of Beirut's Hospitals
- Jabak Receives the New Ambassador of the Order of Malta
- Jabak's Media Office: A Beauty Salon Sealed with Red Wax for Carrying out Cosmetic Procedures Illegally
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.473/1 and No.474/1 and No.475/1 Date 20/3/2019
- Happy Mother's Day from MoPH
- Health Tips from MoPH on Mother's Day
- Agreement between Jabak and Abou Faour to Revitalize the Pharmaceutical Industry
- Jabak Launched the Proficiency Testing Training Project under the AMR Program
- About the PSO
- Work Program
- Functions
- Mission
- Background and Rationale
- Launching of the Statistical Bulletin 2017
- Guiding Committee
- Office of Jabak: The Job Announcement Allegedly Published by the Ministry of Public Health is False
- National Colon Cancer Awareness Campaign 2019
- Launching Event of "Comprehensive Primary Care towards Universal Health Care" at the Grand Serail
- Media
- TV Spots
- Launching Event of "Comprehensive Primary Care towards Universal Health Care" at the Grand Serail
- Trainings for PHC Staff
- Primary Healthcare Projects and Programs
- B-Population and Vital Statistics
- Jabak Received a Delegation from the Lebanese University and Followed up the Health Risks of Pollution
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.368/1 Date 11/3/2019
- Jabak Meets with the World Bank Regional Director Saroj Kumar
- MoPH Pricing of Medicines: Here are the Facts
- Jabak: We will Maintain the Financial Ceilings of the Private Hospitals and Make them Unlimited for the Governmental Ones
- Jabak from Tripoli : I will Raise the Financial Ceiling of Tripoli and Orange Nassau Governmental Hospitals. Any Hospital that Denies a Patient Admission to the Emergency Room won't Go Unpunished
- Jabak Excluded the Possibility of the U.K. 's Decision having Implications on the Ministry of Public Health
- Jabak and Najjari Discussed the Cooperation between Lebanon and Egypt in the Exchange of Medicines
- Al- Fanar Hospital's Patients Moved to Medical Centers in Tyre and Jwayya
- The Health Committee Transferred Patients from Al-Fanar Hospital to Imam Al-Kazem Center and Jwayya Hospital
- Jabak Denounced the Attack on Dr. Abou Shami: The Perpetrators Should be Identified and Held Accountable
- Jabak Met with a Delegation from the Alliance of Palestinian Forces and Promised to Reduce the Prices of Medicines by 80%
- List of Food Supplements Permitted By MOPH
- Hasbani Signed the Renewal of the Cooperation Agreement with the French Blood Establishment: We Constantly Work to Improve the Health Sector
- Good Governance for Medicines and Quality Assurance Programmes
- Good Governance Program in Lebanon (GGM)
- Jabak Took Part in the Council of the Arab Ministers of Health: We cannot Remain Impassive in the Face of this Deplorable Situation
- The Ministry of Public Health's Clarification about the Coverage of Medical Exams at Hariri Hospital
- Jabak Takes Part in the Council of Arab Ministers of Health's Meetings in Cairo
- National Health Accounts 2015
- NCR tables - Distribution by histopathology findings
- Minster of Public Health Discussed with the Iranian, French and Korean Ambassadors the Situations
- National Campaign for the Screening and Early Detection of Heart Diseases 2019
- Launching of National Campaign for the Screening and Early Detection of Heart Diseases 2019
- F-Diseases’ Surveillance Data
- I-National Health Accounts
- Table of contents
- Acknowledgments
- H-Medication for Chronic Illnesses Program: the YMCA Records
- G-Vital Data Observatory “VDO” (previously known as “MNMNS”)
- E-Vaccination and Campaigns
- C-MOPH Services Utilization Data
- A-Summary Tables
- Foreword
- Jabak Discussed with the Syndicate of Hospitals Owners the Health Sector Issues and Received an Invitation to Attend the Arab Hospitals Forum in Cairo
- Jabak Met with the Ambassadors of Turkey and Denmark and Reviewed the Dossiers of the Hospital Establishment in Arsal and Deir El Qamar
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.255/1 Date 20/2/2019
- New Version of Ophthalmology Guideline - 2018
- Jabak Toured Al-Fanar Hospital and Promised to Transfer the Patients to other Hospitals
- Launching of the National Clinical Trials Registry (LBCTR)
- Handover Process at the Ministry of Public Health
- National Health Accounts 2012
- National Health Accounts (NHA)
- Pharmaceutical Products Recalled from the Lebanese Market according toMinister's Decision No.231/1 Date 4/2/2019
- Health Indicators
- New List of Drugs Pricing Reduction from 17/1/2019 till 1/2/2019
- Memorandum No.4 of 6/2/2019 that Calls on the Inspection Doctors to Sign the Patient's Paperworks instead of the TPA's Representatives
- Hasbani Meets with his Saudi Counterpart and the Lebanese Taking Part in the Arab Health Exhibition in Dubai
- MoPH: Closure of Two Unlicensed Beauty Centers in Hadath and Furn el Chebbak
- Revised Hospital Accreditation Standards in Lebanon- January 2019
- Call for Hospital Accreditation Surveyors
- Call for Lebanese Hospitals Accrediattion, Medical Doctors Surveyors
- Children's Cancer Center of Lebanon Launched "I Am And I Will" Campaign
- Lebanon Ranked 23rd in the World for Healthcare Efficiency
- Moph: Prevention Guidance following the Storm Repercussions
- Letter from the Ministry of Public Health to the Ministry of Interior to Inquire about an Association
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.180/1 Date 30/1/2019
- Other Statistics
- Coordination of the Joint Program and the Universal Health Coverage Programs
- MoPH: the Sweden's Offer to Sell Lebanon Cancer Drugs, a Lie
- Our Vision / Mission
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.145/1 Date 25/1/2019
- Hasbani: Drugs are Bought by the Moph more Cheaply or at the same Price than the Ministry of Defense
- جدول بالقيود المفروضة من قبل وزارة الصحة العامة
- Meeting of the National Committee of the Observatory for Maternal and Neonatal Mortality
- Medicines and Medical devices
- Hasbani Calls on Tueini to Target the Real Corruption Cases
- Hasbani Reminded Hospitals to Accept Emergency Cases even if Payment is not Provided
- MoPH Explains what Happened at Al Makassed Hospital
- Lebanon Ranks First in the Arab World as to its Performance in Health Sector
- Hasbani Meets Representatives of the International Organizations and the Donor Countries
- MoPH: "Al-Akbar" Newspaper Tarnishes again its Credibility by Spreading False News
- Hasbani Closes the Nurseries in Beirut Friday
- MoPH: Atris Received Treatment in the Hospital at our Expenses. We Call on the Residents to Respect Traffic Laws
- Drugs Public Price List 2016
- Drugs Public Price List 2017
- Drugs Public Price List 2018
- Drugs Public Price List 2017
- Drugs Public Price List 2016
- Hasbani Forms a Committee to Implement the Infrastructure of the Health Care Card
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.74/1 Date 15/1/2019
- Hasbani Visits the Patient who Underwent the First Lung Transplant Surgery in Lebanon at AUBMC
- MoPH: Parents shall Decide whether or not to Send their Kids to the Nurseries
- Moph: A Dispensary Closed at Wadi El Zayni
- MoPH Closes a Medical Clinic on Hadi Nasrallah Highway and withdraws the Licenses of Two Doctors
- Mental Health and Psychosocial Support Indicators
- MoPH Calls on the Nurseries Located at Areas 700 m and up to Close Tuesday
- Useful Links
- MoPH Calls on the Nurseries to Close Wednesday because of the Storm
- Health System Response
- Health Status
- MoPH Closes Medical and Beauty Clinics Employing Turkish Doctors
- Hasbani from Bkerki: We Want a Government Able to Take Bold Decisions
- Health Determinants and Risks
- Hasbani Announced that Seven Factories had been Referred to the Public Prosecutor for Using the Banned Rhodamine B
- Hasbani Highlights the MoPH's Services and Accomplishments in 2018
- Moph: The Amounts Due to Hospitals were Transferred to the Ministry of Finance for Payment
- Hasbani Visits Audi: The Government Formation Process is Carried out with Good Intentions
- Hasbani at Karatina Governmental Hospital after Turing it into a University Hospital
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.2662/1 and No.2663/1 Date 26/12/2018
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2623/1 Date 21/12/2018
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2622/1 Date 21/12/2018
- Hasbani Launched the National Policy on Infant and Young Child Feeding
- MoPH: The Palestinian Child Wehbeh Received Treatment at the Expense of UNRWA and was Admitted to the Hospital as Required
- European Union support for the Lebanese Healthcare System reaches €173 million
- European Union support for the Lebanese Healthcare System reaches €173 million
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2543/1 Date 14/12/2018
- Strategic Plan for the Medium Term (2016 to 2020)
- Universal Health Coverage Day 2018
- Hasbani Inaugurated the Nuclear Imaging and Radio Therapy Department at Tripoli Governmental Hospital
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2522/1 Date 11/12/2018
- EPI Multi Year Plan of Action 2017-2022
- Orientation Sessions for Rationalizing the Prescription of Psychotropic and Neurological Medications
- Ministry of Public Health Strategy: "Health 2025"
- The Regional Parliamentary Working Group on Universal Health Coverage in the Eastern Mediterranean Region Started its Work in Beirut
- MoPH: the Ministry's Doctor has Performed his Duties to the Fullest as to the Deceased Passeger
- The UCL–Lancet Commission on Migration and Health: the health of a world on the move
- The MoPH Arrests a Man for Posing as Doctor and Seals an Apartment in Zouk Mosbeh with Red Wax
- Hasbani Meets with a Delegation of the World Health Organization
- Hasbani and Foucher Discuss the Repercussions of the Delay in the Formation of the Government on the Decisions of CEDRE Conference and the Support of the Health Sector
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2361/1 Date 21/11/2018
- Hasbani Launched the National Awareness Campaign on Iron Deficiency
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decisions No.2307/1 & 2312/1 Date 16/11/2018
- Hasbani Temporarily Appoints Aoun as Chairman of the Board of Directors of Jezzine Hospital and Assigns Massad as Director
- Hasbani Meets with the World Bank Delegation and the Funding Agreement Brought into Operation
- Several Laws Related to Health Passed by Parliament
- Closure of a Pharmacy in Sin el Fil
- MoPH Confirms that Rhodamine B Substance is not Registered in the Ministry of Public Health
- Press Release in Response to "Al Akhbar" Newspaper Concerning Chebaa Governmental Hospital
- Hasbani Announces MoPH Coverage of Out-Patient Services by 70% in Public Hospitals
- Good News for all Lebanese citizens: The Adoption of the Draft Law on Health Card Fully in the Finance and Budget Committee
- NCR tables - Introduction
- Resources
- Surveillance
- System Overview
- Reform Measures Taken by Jezzine and Chebaa Governmental Hospitals
- Hasbani's Lecture on "the Role of Deputy Prime Minister"
- Launching of the National Electronic Cancer Registry
- Launching of the National Electronic Cancer Registry
- NCR graphs - Distribution (%) by site
- NCR graphs - Introduction
- Distribution of the WHO World No Tobacco Day 2018 Award to Dr. Fadlo R. Khuri President of the AUB
- Célebration des 10 Années de Coopération avec la France
- Global Conference on Primary Health Care
- Press Release Concerning Aids Infection
- MoPH Issued a Clarification Concerning the Drugs Prices Difference Compared to Turkey
- Hasbani Laid the Foundation Stone for the Construction of a PHC center in Sheikh Taba Akkar
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2160/1 Date 29/10/2018
- Key Facts
- Generalities
- System Overview
- NCR tables - Introduction Reporting Forms
- Guideline
- Official Texts
- NCR tables - Introduction Surveillance Data
- Surveillance
- Presentations
- Case Studies
- Brochures and Posters
- Resources
- Key Facts
- Generalities
- System Overview
- NCR tables - Distribution by histopathology findings Reporting Forms
- Guideline
- Official Texts
- NCR tables - Distribution by histopathology findings Surveillance Data
- Surveillance
- Presentations
- Case Studies
- Brochures and Posters
- Resources
- Key Facts
- Generalities
- System Overview
- NCR tables: Distribution of cases by age and site Reporting Forms
- Guideline
- Official Texts
- NCR tables: Distribution of cases by age and site Surveillance Data
- Key Facts
- Surveillance
- Generalities
- Presentations
- System Overview
- Case Studies
- NCR tables: Distribution of cases by age and site Reporting Forms
- Brochures and Posters
- Guideline
- Resources
- Official Texts
- NCR tables: Distribution of cases by age and site Surveillance Data
- Surveillance
- Presentations
- Case Studies
- Brochures and Posters
- Resources
- Key Facts
- Generalities
- System Overview
- NCR tables - Counts of cases Reporting Forms
- Guideline
- Official Texts
- NCR tables - Counts of cases Surveillance Data
- Surveillance
- Presentations
- Case Studies
- Brochures and Posters
- Resources
- Key Facts
- Generalities
- System Overview
- NCR tables - Counts of cases Reporting Forms
- Guideline
- Official Texts
- NCR tables - Counts of cases Surveillance Data
- Surveillance
- Presentations
- Case Studies
- Brochures and Posters
- Resources
- Key Facts
- Generalities
- System Overview
- NCR graphs - Distribution (%) by site Reporting Forms
- Guideline
- Official Texts
- NCR graphs - Distribution (%) by site Surveillance Data
- Surveillance
- Presentations
- Case Studies
- Brochures and Posters
- Resources
- Key Facts
- Generalities
- NCR graphs - Age specific incidence rates Reporting Forms
- Guideline
- Official Texts
- NCR graphs - Age specific incidence rates Surveillance Data
- Presentations
- Case Studies
- Brochures and Posters
- Key Facts
- Generalities
- System Overview
- NCR graphs - Incidence rates by site Reporting Forms
- Guideline
- Official Texts
- NCR graphs - Incidence rates by site Surveillance Data
- Surveillance
- Presentations
- Case Studies
- Brochures and Posters
- Resources
- EPI Techical Committee Meeting 18/10/2018
- Honoring from "Khirbet Qanafar” Governmental Hospital to HE Minister Ghassan Hasbani
- On the World Polio day, the Lighting of the National Museum under the Patronage of the Minister of Health
- The Head of the Board of Directors of the “Jezzine” Governmental Hospital was Suspended from Work
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2144/1 Date 25/10/2018
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2140/1 Date 25/10/2018
- Hasbani Discussed with AFD Delegation the Establishment of the Central Laboratory and the Support of the Governmental Hospitals
- Hasbani: Until the Last Minute we Will Follow the Health Card Law in the Committees of the Council
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.2106/1 Date 23/10/2018
- Hasbani Launched a Live Maneuver to Counter Chemical Attacks
- MoPH Celebrating the International White Cane Day
- Hasbani Announced Elissa Ambassador of the Breast Cancer Awareness Campaign
- 31 May: World No Tobacco Day 2017
- National Campaign for Screening and Early Detection of Heart Diseases 2018
- National Awareness Campaign on Sudden Cardiac Arrest in Young Athletes 2018
- Hearing Screening National Awareness Campaign 2018
- Hasbani Concluded the Activities of the Youth Camp and the 2030 Vision Competition and Called for Investment in Sustainability
- Policy Support Observatory (PSO)
- Hasbani Launched the National Children Obesity Awareness Campaign
- The National Children Obesity Awareness Campaign 2018
- National Mental Health Awareness Campaign 2018
- Launching of the Policy Support Observatory at the MoPH in Partnership with the WHO and AUB
- The Policy Support Observatory Holds its Second Guiding Committee Meeting to Discuss the Work-Program
- MoPH Organizes Two Training Sessions for Radiology Technicians in Preparation for the Launch of the National Breast Cancer Awareness Campaign
- Those Claiming the Increase of the Governmental Hospitals Ceiling are Secretly Demanding the Increase of their Private Hospital’s Ceiling. We will Continue to Reduce Drugs’ Prices
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1914/1 Date 10/10/2018
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1902/1 Date 9/10/2018
- Mental Health Awareness Campaign 2018
- Hasbani Presided over the First Meeting of the Policy Support Observatory Guiding Committee to Discuss Priority Areas for the PSO Work Plan
- Hasbani Headed the Supreme Health Council: We will not Stop Planning for the Future of the Health Sector even if the Government is in a Caretaking Capacity
- Hasbani Met with the Board of Directors of Jezzine Governmental Hospital and Communicated with the Central Inspection to Speed up Procedures
- Hasbani Delivered Official Documents to Ibrahim who Closed the File of Ministry of Public Health
- Referring a Pharmacy to the Public Prosecution because it Sells Milk Distributed Free of Charge by MoPH
- "Participatory Governance of Solidarity with the Public Sector" a New Article on "An-Nahar"- Dr. Walid Ammar
- Guide for the rational prescription of medications for priority mental and neurological conditions for specialists in the public health system
- Food Supplement Recall from the Lebanese Market
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1867/1 Date 1/10/2018
- Hasbani to “Al Iktissad wal Aamal”: The Crises Besiege Lebanon and Require Difficult Decisions and the Economic Situation cannot Wait for Oil and Gas Revenues
- National Mental Health Awareness Campaign 2017
- The Violations of Jezzine Governmental Hospital have been Transferred to the Central Inspection since July 2018
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1805/1 Date 26/9/2018
- Mental Health: Call for Public Hospitals-Academia-Civil Society Organizations Partnerships
- Hasbani: Stressing that Cancer Medicine is a Humanitarian Issue and the Pain of People is more Important than all of us
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1796/1 Date 24/9/2018
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1738/1 Date 18/9/2018
- Hasbani Launched the Mental Health Awareness Campaign
- Hasbani: the NSSF Operates under the Supervision of the Ministry of Labor. It should Assume its Responsibilities towards its Patients without Referring them to the MoPH
- Hasbani Discusses with the Parliament's Finance and Budget Committee the Medical Card Draft Law
- Hasbani Presented the International Funding for Health Project, the Foreign Affairs and Emigrants Committee Endorses the Law
- The Collaborative Governance of Lebanon’s Health Sector
- The Director General of Health Heads Lebanon's Delegation to the Ministerial Conference on the Road to Achieving Universal Health Coverage in the Eastern Mediterranean Region
- Two Letters from Hasbani to the Ministry of Energy and Water and the Governor of Akkar after Ain Al Zahab Water in Akkar had been Confirmed to be Polluted
- Workshop to Improve Cause of Death Statistics
- MoPH Warns again against the Exposure to Dogs' Bites and Calls on the Concerned Parties to Meet their Responsibilities and Take Precautionary Measures
- Hasbani: The Control on Governmental Hospitals Helps Enhance their Performance
- Ghassan Hasbani
- MoPH Warns again against the Danger of Catching and Consuming Toxic Lagocephalus spadiceus
- MoPH Warns against Buying Contact Lenses or Solutions Posted on Social Media without Obtaining the Required Licenses
- Hasbani during the Opening of a PHC Center at the BAU: We will Continue to Enhance the PHC Network for it Helps Reduce Burdens
- Hasbani’s Office to Boustani: the Government wasn’t a Caretaker Body in 2017
- MoPH: The Social Media’s Misreporting of Deaths Tarnishes Lebanon’s Image
- Newsletter
- Hasbani: The Disease cannot Wait for the Formation of the Cabinet
- MoPH Shuts down a Restaurant, a Supermarket and a Slaughterhouse and Recalls a Product
- Hasbani Briefed the Health Committee on the State of Health Sector
- Hasbani: The Information Concerning Arwan Industries' Expired Medicines being Circulated in the Market is Groundless
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1601/1 Date 28/8/2018
- Rabies Prevention and Control
- Hasbani: We have Asked to Transfer Funds Amounting to 10 Billion Pounds for the Completion of Deir El Qamar Hospital, but it wasn’t Placed on the Cabinet’s ِAgenda
- MoPH Calls on the Energy and Water Ministry to Identify Polluted Sea Areas and Take Measures according to Law No. 77/2018
- MoPH: There is no Carcinogenic "Rice" in Lebanon as Claimed by some Syrian Media
- Reception and Implementation of the Japanese Grant of over USD 4 million to 14 Governmental Hospitals
- Al Asmar and the Governmental Hospital Employees Thanked Hasbani for the Salary Scale
- A Warehouse of Medicines Raided in Damour by Lebanese Customs; the MoPH not Being Informed
- "MoPH" Condemns the Attack on Hospitals, "St. Georges" and "Universal" and Demands the Judiciary to Issue Strict Sentences "
- MoPH Summons the Company Importing Brucellosis Medicine to Inquire about its Unavailability in the Markets
- Subscription to esumoh mailing list
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1567/1 Date 10/8/2018
- Subscription to esumoh mailing list
- A Comprehensive Survey of the Governmental Hospitals Conducted in Cooperation between the MoPH and the Central Inspection
- Hasbani Halts AB Slim Circulation
- Campaigns were Conducted against the Ministry because of its Minister's Stances; some Dossiers were Excluded from the Cabinet's Agenda
- Chemical Surveillance
- Classical reporting system
- Hasbani Launched Hearing Screening National Awareness Campaign
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1378/1 Date 17/7/2018
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1452/1 Date 31/7/2018
- Minister Hasbani’s Visit to Bkerki
- New Minister Decision No. 1424 date 27/7/2018 Concerning the 2D Matrix Barcode Implementation
- MoPH: "It is not True that Tetanus Injections are not available in the Lebanese Markets"
- Hasbani Announced the First Successful Uterus Transplant in Lebanon and the Middle East at Bellevue Hospital
- Hasbani Concluded his Visit to New York with Meetings with UN Officials and Ambassadors
- The MOPH Condemns the Attack on the Chief of ER at Hotel Dieu Hospital and Calls on the Public Prosecution Service to Take Action
- Hasbani Presented Lebanon First Report on UN Development Goals
- National Report on Drug Situation in Lebanon – 2017
- Hasbani Delivered the ESCWA Statement at the UN Political Forum the Sustainable Management of Natural Resources is a Must
- Lebanon among the World Countries that have Made the Most Progress in PHC
- Pharmaceutical Products Recalled from the Lebanese Market according to Minister's Decision No.1376/1 Date 16/7/2018
- MoPH: Toxins in Breastfeeding Milk in Lebanon are within WHO Normal Rates
- Publications of the National Observatory on Drugs and Drug Addiction (NODDA)
- Hasbani to Head a High-Level Lebanese Delegation to the UN Political Forum
- "3a Stouh Beirut Association" Briefed on How Donations will be Allocated
- Hasbani Discusses with the Lebanese Syndicate of Medical Laboratories the Matters of the Sector
- National ِAwareness Campaign Against Drugs 2018
- The Minister of Public Health Discussed with a Delegation from North Lebanon the Health Impacts Caused by Neglect of Pollution Treatment
- Launching of 2018 Vaccination Campaign for Pilgrims
- Hasbani Sponsored a Competition for Outstanding Students
- MoPH:No Shortage of Drugs for Cancer and Incurable Diseases; they are Constantly Being Delivered in Quarantine
- Lebanon Clinical Trials Registry Training
- Hasbani Launched "Lebanon without Drugs or Addition" campaign
- Hasbani and Adwan Laid the Foundation Stone for Damour Medical Center
- National Observatory on Drugs and Drug Addiction
- Hasbani during the Inauguration of an Advanced Division at the Radiotherapy Department of Mount-Lebanon Hospital
- Audi Commended Hasbani's Fair and non-Politicized Approach to Financial Ceilings
- Hasbani Presided over the Meeting of the National Committee for Sustainable Development at the Grand Serail
- Hasbani from Rmeish: We Demand the Return of the Syrian Refugees to their Country and the Repatriation of the Lebanese Deportees from the Occupied Territories
- Al-Jeser Visited Hasbani: The Financial Ceiling for Tripoli's Hospitals Should be Increased and the Slaughterhouse's Functioning Should Abide by its Specific System
- Warning from MoPH to the Nursery that Rejected a Sudanese Kid and Racism Awareness Sessions to be Conducted in Cooperation with the Social Affairs Ministry
- Hasbani and Khalil Signed a Decree to Allocate LBP 10 Billion Treasury Loan for Rafic Hariri University Hospital
- Hasbani during the EU's Launching of Two Health Care Projects that Constitute a First Line of Defense for Public Health and the Prevention of Epidemics
- Minister Hasbani Receives the Support of the Maronite Synod
- The Minister of Public Health Responds in a Press Conference to the False Accusations Regarding Drugs' Pricing in Lebanon
- Hasbani: the Financial Ceiling for each Hospital was Fairly set and the Major Problem Lies in the Non-Payment of Arrangement ِِAgreements since 2000"
- MoPH Confirms its Support to Tripoli Hospitals and the Increase of the Total Financial Ceiling for 2018
- Salary Scale for Governmental Hospital Employees soon to be issued
- Laboratory Technician Competence Exams for Students Applying for Professional Practice License
- Open Day in Hotel Dieu to Raise Awareness of Smoking-Related Risks
- MoPH Participation in the 71th World Health Assembly in Geneva
- The MoPH National Committee for Communicable Diseases: All Reports and Analyses Confirm that there is no Epidemic Outbreak in Kfarabida
- The MoPH Follows up the Situation in Kfarabida and Confirms that there is no Epidemic Outbreak
- Saint George Hospital University Medical Center Opened the New Nuclear Medicine Center
- Hasbani during the Ceremony Honouring the Memory of the Deceased Pr. Khaled El-Mohtar
- Hasbani Launches a Cooperation Programme with Hôtel-Dieu de France in Radiotherapy
- Hasbani and Audi Brought up the File of Saint George University and the Need to Endorse it
- Hasbani Opens the Regional Conference on Osteoporotic Fractures Prevention
- Hasbani Sponsors a Conference on Skin Diseases and Emphasizes the Need to Maintain Ethics
- The 71th World Health Assembly
- Hasbani Informs the Governmental Hospital Employees of the Cabinet's Decision on their Inclusion in the Salary Scale and the Delegation Apologizes for Abuses
- Health Awareness Workshop for the Fasting at MoPH and Medical Advice for People with Diabetes and High Blood Pressure
- Hasbani after Meeting Audi: the License Approved to Establish Saint George University in Beirut is a Major Step and Adds Great Value to Education
- Health Tips for Fasting
- National Awareness Campaign on Thalassemia Prevention 2018
- Hasbani and Dabbousi Signed a Memorandum of Understanding between the MoPH and the Chamber of Commerce, Industry and Agriculture - Tripoli
- Hasbani Representing Aoun on the Opening of the Order of Nurses Conference
- Ammar Representing Hasbani during The launching of the National Plan for Awareness and Early Detection of Colon Cancer
- Food Supplements Committee
- Hasbani Opened the Health Forum in its Second Edition and Presented the Achievements of the Ministry in 500 Days
- Awareness Campaign on Thalassemia Prevention
- The MoPH Won the 2018 Award for Excellence and Distinction in PHC
- Arwan National Biotechnology Product Launched under the Patronage of Hasbani
- The MoPH Follows Scabies Cases among Syrians in Abra Public School
- Workshop for "Health" in Cooperation with the European Union-TAIEX to Promote National Pharmaceutical Industries
- On World Immunization Week 2018 MoPH: We are all Responsible for Protecting our Children through Vaccination
- Public Tender for Drugs for the Ministry of Public Health
- Hasbani Calls on the Cabinet to Adopt a Mechanism for Determining the Financial Ceilings of Hospitals
- The MoPH Cautions against the Risk of Death from Mushrooms, Wild Herbs and Toxic Fish
- Hasbani during the Launching of the 7th Pharmacy Conference at the USJ: A Noble Profession and Mission that Embody Human and Social Values
- Universal Health Coverage: Bridging the Gaps
- Helou Representing Hasbani on World Tuberculosis Day: We Commit to end this Epidemic by 2030
- Non-Communicable Diseases
- Hasbani Demands the Immediate Implementation of the Salary Scale Law for the Governmental Hospital Employees in the Cabinet
- Vaccination and Awareness Campaigns Conducted by the Ministry of Health against Measles
- MOPH Warns Against Measles Outbreak in Lebanon and Assures It will Secure Vaccines Free of Charge
- Additional Vaccines Requested as a Precautionary Step. Hasbani: "We have Conducted the Necessary Campaigns with the UNICEF to Control Measles"
- "The National Registry for Hemophilia" Launched by Hasbani. I will Work with the HC Payor to Enhance the Treatment Services
- MoPH Warns against the Increasing Number of Dogs' Bites Victims and the Severe Global Shortage in Vaccines
- Cost of Oncology Drugs in the Middle-Eastern Country of Lebanon: An Update (2014-2016)
- Launching of the Policy Support Observatory: MOPH-WHO-AUB Partnership Monday 16 April, 2018 (Closed Event)
- Panel Discussion, World Health Day 2018, WHO EMRO, Cairo, April 4th 2018
- Health Minister Launches the Second Session of the Future Health Forum with the Participation of IDAL and Libanpost
- Hasbani:"We are not Going to Allow the Registration or Import of Items Harmful to the Health of the Lebanese"
- Award of Appreciation from MoPH to Dr Michael Woodman
- World TB Day 2018
- Two Memoranda of Understanding Signed between the MoPH, AUB and USJ under the Patronage of Hasbani
- Lebanon Officially Nominates Dr. Rana Hajjeh for the Post of WHO Regional Director for the Eastern Mediterranean
- Hasbani Visited the Sextuplets and their Mother at St. George's Hospital
- Nature Podcast on Global Mental Health
- Documentary: "Mental Health in Lebanon: Vision and Achievements"
- Episode 1 of the “Ask the Policy Expert” Webinar Series with the head of the National Mental Health Programme
- Hasbani Launches the Supreme Health Council
- Health Ministry Publishes Drug Price Index and Ensures the Reduction of Prices
- Issuance of Director General Circular Number 22 Date 9/3/2018 Related to the Regulation of Studies and Research in the Field of Mental Health and Psychosocial Support
- Press Conference on Stray Dogs Phenomenon that Threatens the Health and Safety of the Citizens
- Ceremony in Support of Children with Cancer at the MoPH with the Participation of the Voice Kids Stars
- Japanese Medical Equipment Delivered to Hariri Hospital. The Japanese Ambassador Affirmed his Country's Continued Support to Lebanon
- Hasbani Meets with a Delegation of the Order of Pharmacists. "Reforms Should be Immediately Implemented"
- Health Ministry: Medicine Prices Reduction Reaches 70%
- Hasbani's Office: "The Supreme Council of Health has been Established since October and Said is four Months Late"
- Health Ministry Calls on the Municipalities to Promptly Find a Solution to the Phenomenon of Stray Dogs
- Hasbani Launched the National Campaign for the Prevention of Cardiovascular Diseases: No.1 Cause of Hasbani Launched the National Campaign for the Prevention of Cardiovascular Diseases: No.1 Cause of Death in Lebanon
- Rabies
- Launching of the National Awareness Campaign on Sudden Cardiac Arrest in Young Athletes
- National Vaccination Campaign 2017
- National Campaign Against Diabetes 2017
- The Cleft Lip National Awareness Campaign 2018
- Heath Minister Discusses with the Minister of Finance the Inclusion of the Governmental Hospitals Employees in Salary Hike Progress Achieved in this Regard
- Representatives of the Governmental Hospital Employees Met with Director General Dr. Walid Ammar and Officials in Health Ministry
- Governmental Hospitals Employees Sit-in Suspended Hasbani: We are Working to Develop Appropriate Frameworks for the Implementation of the Salary Scale
- Press Release on Mobile Application “Ballegh Lalsoha”
- Hasbani: We are Pursuing our Efforts to Finalize the Project of Establishing Deir al-Qamar Governmental Hospital
- Hasbani Launched the Cancer Treatment Guidelines
- Hasbani during the Workshop on Genetic Testing: the Country Cannot Continue without the Rule of Law
- Hasbani and the UNICEF Launched the National Breastfeeding Campaign
- The Ministry of Public Health Pursues its Efforts to Include the Governmental Hospitals Employees in Salary Hike
- Hasbani from Dubai: Public-Private Partnership in Hospitalization Sector Opens New Horizons for Development where the Patient is the Major Beneficiary
- Hasbani Presents Shocking Figures and Rings the Alarm Bell: Stop Waste Burning
- National Breastfeeding Campaign 2018
- Walid Ammar dans l’Ordre de la Couronne Belge- L'Orient Le Jour
- Information, Education and Communication material
- Press Release in Response to Newspaper Article about "Insane Persons Running Away from Hospital"
- Issuance of a New Drugs Public Price List
- Medical Technology
- Lebanon Ranking First in the Arab World and We Encourage Investment in the Healthcare Sector
- Intensive Meetings at Health Ministry with the Governmental Hospitals Workers
- MoPH Warning: The Precautionary Guidelines for Rabies Control must be Complied with
- Hasbani from Davos: The Stability and Institution-Building are Key to Investment in Reconstruction
- Meeting to Discuss the Principles of Governance for the Pharmaceutical Profession in Lebanon
- Health Ministry Launched a Workshop to Introduce the European Standards for the Pharmaceutical Industry in Collaboration with the EU
- Issuance of a New Drugs Recall Resolution No.161/1 Date 24/1/2018
- Inter-Ministerial Substance Use Response Strategy for Lebanon 2016-2021
- Launching of the National Campaign for Early Detection of Primary Immune Deficiency
- Issuance of a New Drugs Public Price List
- Issuance of a New Drugs Recall Resolution No.124/1 Date 19/1/2018
- Hasbani during the Inauguration of a Center for the National Organization for Organ and Tissue Donation and Transplantation
- Hasbani: I will Remain Committed to the Humanitarian, National and Legal Standards
- Hasbani: We Developed a Comprehensive Health System so as not to Exclude any Citizen from the Universal Coverage
- Issuance of 2 New Drugs Recalls Resolutions No.107/1 and No.110/1 Date 16/1/2018
- Hasbani and Zeaiter Discussed the Agricultural Pesticides in the Ministry of Public Health and Immediate Measures Taken
- Workshop at the Ministry of Health on the Regulation of the Marketing of Infant Feeding Products
- G-Vital Data Observatory “VDO” previously known as “MNMNS”
- Issuance of the Minister Memorandum No.4 of 11/01/2018 Regarding the Implementation of the Memorandum of Understanding Signed with the Lebanese Customs Department
- Hasbani Launched the National Awareness Campaign on Congenital Malformations of the Oral Cavity
- Dr. Ghassan Issa Honoured
- Issuance of a New Drugs Recall Resolution No.73/1 Date 10/1/2018
- Hasbani from Jbeil: The Region has Faced a Significant Shortage in the Healthcare Services and we Work Hard today to Improve its Healthcare Centers
- Issuance of a New Drugs Public Price List No.18/2/35 Date 9/1/2018
- Issuance of a New Drugs Public Price List No.18/2/35 Date 9/1/2018
- Hasbani: What we Need is Partnership not Allocation of Benefits, and Bringing the Foreign Conflicts to Lebanon is Unacceptable
- Hasbani: The Shortage of Some Drugs at the End of 2017 was Solved with the use of 2018 Budget and more Funds should be Allocated to Drugs, Given the Steady Rise in Demand for them
- Consultative Meeting on Reducing the Consumption of Table Salt in Lebanon
- Issuance of 2 New Drugs Recalls Resolutions No.11/1 Date 2/1/2018 and No.22/1 Date 3/1/2018
- Hasbani: Building a Strong State is Based on The Application of The General Accounting Act
- MoPH Circulated to Hospitals to Admit all Emergency Cases
- Ammar at the Annual Dinner of the Laboratory Owners : The Ministry of Health Strives to Provide Excellent Service to Patients
- Hasbani: Lebanon is a Fountain of Thought and Language, and we Hope that it Will be Poured out and Will not be Left Behind
- Hasbani Withdraws the French-made Lactalis Infant Milk from the Lebanese Markets
- Lauching of the Guideline for Good Storage & Distribution Practices of Food Supplements in Lebanon
- Press Release to Hospitals Related to the Security Companies Behavior
- Hasbani Participated in the Conference of Health Ministers of the Organization of the Islamic Cooperation in Jeddah
- Announcement Regarding the Implementation of 2D Data Matrix Barcode on Pharmaceutical Products
- Issuance of a New Drugs Public Price List No. 17/2/47162 Date 11/12/2017
- Collaboration between MoPH and The Lebanese Women Democratic Gathering to Raise Awareness about the Dangers of Child Marriage
- Closure of Dr. Dany Tannous Clinic in Dora
- Closure of Dr. Dany Tannous Clinic in Dora
- Closure of Dr. Dany Tannous Clinic in Dora
- Closure of Dr. Dany Tannous Clinic in Dora
- Hasbani Examined the Reasons behind Hweila's Death in the Lebanese Canadian Hospital:"Justice will Take its Course and we Should Maintain the Public Order"
- No Indulgence with any Staff Proven Corrupted
- Hasbani Asked the Public Prosecution to Conduct the Necessary Investigations and Determine the Responsibilities that will be Built on the Question Requested
- Hasbani Urged the Judiciary to Expedite the Processing of Cases, Announced Additional Actions to Regulate the Work of Specialized Hospital Centers, Addressed the Pharmacist's Case and Stressed that the Ministry of Public Health is the Spearhead for Maintaining the Safety of Citizens
- Press Release Concerning Cases of Poinsoning in the North and the Death of a Child
- Hasbani: We have Taken Several Steps to Control the Healthcare Bill and We have Asked for Additional Funding to Cover the Chronic Diseases
- D-Epidemiology
- Acknowledgments
- B-Population Data and Vital Statistics
- I-National Health Accounts
- E-Vaccination and Campaigns
- C-MOPH Services Utilization Data
- A-Summary Tables
- Table of contents
- Preface
- H-Medication for Chronic Illnesses Program: the YMCA Records
- Issuance of a New Drugs Recalls Resolutions No.2314 Date 1/12/2017
- Issuance of a New Drugs Recalls Resolutions No.2312/1 Date 1/12/2017
- Hasbani in a Visit to Jebbit Bsharri: We Believe in Transparency and Work to Improve the Performance of Institutions and the Role of the Private and Governmental Hospitals
- Réunion en France du Comité Interministériel de Santé
- Issuance of Memorandum No. 133 Concerning the Amendment of Memorandum No. 13 Related to the Implementation of the One Stop Shop
- Issuance of a New Drugs Public Price List No. 17/2/45324 Date 29/11/2017
- Fouad Maksoud Greeted by Hasbani at the Airport: Lebanon is a Main Source of Innovation
- Hasbani: To Develop a Policy that Prevents the Giving of Antibiotics without a Prescription
- Hasbani Pursues his Visit to Jbeil: the Healthcare System is in a Perfect Condition in Spite of the Modest Means
- Medical Devices
- Hasbani in Jbeil: The Situation is Critical and Lebanon is at a Crossroads. The Cohesion is a Must and we Have always Been Working to Preserve the Sovereignty and Independence of the State
- Letters to the editor- Lancet Journal - on the Syrian crisis and mental health system reform in Lebanon
- Hasbani Met in Moscow with Putin's Envoy to the Middle East and the Imperial Orthodox Society Council
- Assessment of mental health and psychosocial support services for Syrian refugees in Lebanon.
- WHO-AIMS Report on Mental Health System in Lebanon 2015
- Hasbani: We Hope To see The Beginning of The End of The Waste Crisis Instead of Temporary and Partial Solutions
- IBloodlink Honours Health Minister. Hasbani: the Ministry Supports the Culture of Blood Donation
- Hasbani after Meeting Archbishop Hilarion in Russia: The Church's Support to the Social Stability and Impartiality are Essential for Lebanon
- test private area
- On World Diabetes Day the Ministry of Public Health Building has Been Lit in Blue under the Auspices of Hasbani
- Free Medical Examination Campaign at the Premises of the Ministry of Public Health during the World Diabetes Day. Hasbani: Awareness is Vital for the Prevention of Disease Complications
- Dr. Joseph El Helou Receives an Award
- Hasbani launched the National Campaign Against Diabetes
- Hasbani Launched Health Awareness Campaign for Early Detection of Prostate Cancer
- Issuance of a New Drugs Recalls Resolutions No.2155/1 Date 9/11/2017
- The Sixth Annual Conference of Free Minds Opened
- Hasbani Visited a Number of Healthcare Facilities in Riyadh
- Hasbani in Riyadh at the Invitation of his Counterpart Al-Rabiah
- Closure of Non-Licensed Nurseries
- Hasbani after Receiving the Merit Medal: The Scout is Honest and Fair
- Laws & Regulations
- Ministers of Public Health and Social Affairs Launch the Joint Plan Between the Two Ministries
- Hasbani Inaugurated the New Center in Tripoli for the Lebanese Dental Association: We Count on your High professionalism to Continue to Provide the Best Healthcare Services
- Hasbani Visited the Chamber of Tripoli and North Lebanon: with the Public Private Partnership Law, Opportunities Can be Better Achieved
- Tripoli Hospital Receives a Grant from the Embassy of Saudi Arabia. Hasbani: Good Health is a Key to a Solid Society and Economy and a Safe Country
- Arbid Representing Hasbani during the Conference on Biomedical and Clinical Engineering: Clear Controls and Conditions should be Established for Medical Investment
- Hasbani's Information Office: We are Keen to Apply Laws and we Regret that some People have Used the Funds for Citizen's Support to Create Political Tensions
- Media
- Hasbani: The Medical Examinations Have Covered 600 Women so Far and Seek to Intensify the Campaign in the Coming Months for Early Detection of the Disease
- Hasbani during the Launch of the Project for the Development of the Healthcare Center in Deir El Ahmar: We are Working to Apply Technology for the Sake of Hospitalization
- Nouvelles Directives pour une Meilleure Mammographie dans les Hôpitaux Gouvernementaux ("L'Orient Le Jour")
- La Stratégie de Santé Globale 2025 Place le Patient au Cœur de ses Objectifs ("L'Orient Le Jour")
- Hasbani: The Minitry’s Efforts and the TPA’s Work Contributed in Reducing the Number of Cases Exceeding the Financial Ceiling in Private Hospitals by 53%
- Hasbani Called on all Hospitals to Receive Wounded People in Zuqaq El-Blat
- Participation of MoPH in the 15th Annual Global Forum for Temperature Controlled Life Science Supply Chains
- Hasbani Representing the President of the Lebanese Republic: We are Working to Enhance the Capacities of the Public Hospitalization Sector and we Have Made a Significant Improvement
- Issuance of a New Drugs Public Price List No. 17/2/38570 Date 16/10/2017
- Launching of the National Breast Cancer Awareness Campaign 2017 under the Patronage and in the Presence of First Lady
- Developing an inter-ministerial substance use response strategy for Lebanon: process, content and lessons learned
- Hasbani Opened an Emergency Healthcare Department at the Airport: at the Service of Passengers and Visitors 24 Hours a Day
- New Record for Lebanon: Largest Breast Cancer Awareness Ribbon made of 8250 Footballs
- Issuance of a New Drugs Recalls Resolutions No.1877/1 Date 9/10/2017
- Hasbani Addressing "Beirut Marathon" Association: Let's Run against Disease
- Issuance of a New Drugs Public Price List No. 17/2/36964 Date 5/10/2017
- Lebanon: mental health system reform and the Syrian crisis
- Assessments
- Minister Hasbani Issues Warnings to Three Hospitals and Refers the Files to the Public Prosecution, Syndicate of Hospitals and the Order of Physicians and Nurses
- Integration of Malnutrition into Primary Health Care
- Statistical Bulletin 2006
- Statistical Bulletin 2007
- Statistical Bulletin 2008
- Statistical Bulletin 2009
- Statistical Bulletin 2010
- Statistical Bulletin 2011
- Statistical Bulletin 2012
- Statistical Bulletin 2013
- Statistical Bulletin 2014
- The Ministry of Public Health Clarifies its Position on Rumours Regarding the Spread of "Leishmania" in Akkar
- The Ministry of Health is Proudly Announcing Its Attempt to Make a New World Record with the World Record Academy
- National Breast Cancer Awareness Campaign 2017
- Hasbani: The Health Sector Will be at the Heart of the Industrial Revolution
- Statistical Bulletin 2015
- Hasbani: "The Governorates Sessions" will Kick off... The Widest Organizational Operation in the History of Lebanon
- Publications
- Integration of Non-Communicable Disease Services within Primary Health Care
- EPI Achievements
- IRB Authorization Meeting
- Hasbani ِAnnounced a Model for Universal Health Coverage: Benefit the Lebanese, Especially those Who do not Have Another Health Cover
- Hasbani Visiting Jezzine
- Hasabani Discussed with Agabova the Challenges Facing Lebanon, the Region and the File of the Syrian Emigration
- The first Lebanese Lady and the Minister of Health Finalized the Launch of the National Campaign to Raise Awareness about Breast Cancer
- Hasbani Sponsored the Third Forum for Research on Cancer Diseases at St. Joseph University
- Hasbani Discussed with the Ambassador of Qatar the Promotion of Cooperation in the Health and Medicine Sectors
- A Surprise Visit from Hasbani to Marjeyoun Governmental Hospital
- Hasbani from Marjaayoun: This Area is at the Heart of Lebanon's History and Should not be Left Out of the Care of the State ... So We Are Here
- Turning Adversity into Opportunity: the Syrian Crisis and Mental Health Reform in Lebanon
- The “4Ws” in Lebanon: Who’s Doing What, Where and Until When in Mental Health and Psychosocial Support
- Hasbani from Russia: Lebanon's Interest Requires to Spare it from Tensions and Build Economic Bridges
- F-Diseases’ Surveillance Data
- D-Epidemiology
- H-Medication for Chronic Illnesses Program: the YMCA Records
- Acknowledgments
- I-National Health Accounts
- G-Maternal Neonatal Mortality Notification System (MNMNS)
- E-Vaccination and Campaigns
- C-MOPH Services Utilization Data
- Articles
- B-Population Data
- Policy briefs
- A-Summary Tables
- Table of contents
- Minister's Foreword
- Reports
- Table of contents
- Mappings of services
- Mappings of services
- Issuance of a New Drugs Recalls Resolutions No.1685/1 Date 7/9/2017
- Hasbani: Success or Failure of the Covenant is Related to the Conduct of Elections or Not
- The Ministry of Public Health Issues Warnings to 13 Hospitals for Engaging Non-Lebanese Staff
- Issuance of a New Drugs Public Price List No. 17/2/32840 Date 31/8/2017
- Epidemiological Surveillance
- The National Mental Health Programme
- Hasbani Announced the Outcomes of the Services Coordinating Committee's Meetings in the Governorates: The Cabinet Meetings to be Held in the Governorates as of 28 September
- Hasbani Announced the Holding of Beirut International Healthcare Industry Forum in March: To Implement the Recommendations of the First Session to Place Lebanon on the Middle East's Health Map
- MoPH Followed up the Case of Mass Poisoning at a Wedding in Beqaa and the Closure of Two Butcher Shops as a Precautionary Measure
- Hasbani Visited the Healthcare Center in Barqa: State-Building cannot be Achieved in the Light of the Widespread Corruption. Becharreh-Deir El Ahmar Tunnel to be Discussed soon by the Cabinet
- Launching of the New Birth Registry
- Minister Abou Faour Discussed the UNRWA Crisis with the Palestinian Delegates
- Press Conference for HE Minister Abou Faour with the Head of the EU Mission in Lebanon to Launch the 2nd Phase of the “Health System Support in Lebanon” Program
- The Ministry of Public Health Launches the New Standards Guidelines for Mammography
- Hasbani to NNA from Dubai:”We are Working to Achieve the e-Government and Digital Society and the MOPH will Launch very soon the One Stop Shop for Services”
- Hasbani to the Director of the UAE Health Authority :”To Promote Cooperation and Exchange of Health Experiences between the two Countries “
- Inauguration of the New Building for the Lebanese Hospital Geitawi under the Auspices of Patriarch Al-Rai
- Accreditation Criteria for Inpatient Psychiatric Units in General Hospitals
- Hasnabi’s Round in Zahleh Concluded with a Visit to the Al Yassine Medical Center in Taanayel
- Hasbani during the Graduation Ceremony of Sagesse High School Students: Be prepared for the Future, Have Enough Confidence and Fight for what you Believe in
- Hasbani During the Launch of the Higher Institute of Heath in USJ: We are Still Far From Achieving Health Equity
- HE Received a Delegation from Bouar Hospital Staff. Hasbani: I Signed the Payroll To Ensure the Continuity of the Public Facility
- Hasbani Visited Ras Baalbek and Qaa: The Army does not Need to Coordinate with Anyone, as It has Achieved Quality Accomplishments Alone
- Hasbani Visited Al Mahabba Hospital in Deir El Ahmar: North Beqaa is a Priority for the State
- Huge Reception to Hasbani in Deir El Ahmar
- Hasbani Inaugurated a Station for the Distribution of Drugs in Baalbek Hospital: Our Door is Open to Everyone. Al Makdad: It is Important to Establish a Drug Rehabilitation Center to Save our Youth
- Hasbani in a Visit to Baalbek:Hand in Hand to Meet the Needs within the Available Resources. Zaiter: We will Discuss the Needs of the Region during the Cabinet's Meeting that will be Held in Baalbek
- Fifth Annual Congress for the Lebanese Society for Quality & Safety in Healthcare
- Issuance of a New Drugs Public Price List No. 17/2/30899 Date 22/8/2017
- Participation of MoPH in the 15th Annual Global Forum for Temperature Controlled Life Science Supply Chains
- Issuance of a New Drugs Recalls Resolutions No.1562/1 Date 18/8/2017
- Hasbani Inspected a Vaccination Campaign at al Masnaa Border Crossing
- Hasbani Submitted Canadian Survey Reports to Primary Healthcare Centers: We won't Spare any Effort to Support PHC Centers for the Achievement of Universal Healthcare
- Hasbani: Addiction Destroys Humans and Homelands and we will Strengthen the Support of Governmental Hospitals
- Hasbani Visits Audi: To Upgrade State Educational Institutions
- Hasbani: Lebanon is Today very Immune to the Outbreak of Epidemics
- Hasbani has been Briefed by the President of the Arab Hospital Federation on the Preparations for the Arab Health Economic Forum on July 7
- After the Success of the First Pediatric Heart Transplant in Lebanon. Hasbani Checks on the Patient: If There Were no Donor Child, We Wouldn't be Able to Save Another Child
- Hasbani in Hospitals Strategy Workshop: We Work for the Rehabilitation and Equipment of Emergency Departments, the Provision of Training and the Establishment of Emergency Unit
- Hasbani in Preparation for Beirut International Healthcare Industry Forum: We Work to Cover 1.8 million Lebanese without Overstepping the Authority of Insurance Bodies
- Hasbani during the Ceremony of Free Life without Smoking Association: Smoking is a Suicide, a Slow Death for the Smoker and his Surroundings and a Devastating Means
- Development of Medical Specialties, Public Health and Colloquium Examinations in Lebanon
- Meeting of the Committee in Charge of the Implementation of the Medicines Barcode and the Unified Medical Prescription Projects
- The International Musculoskeletal Society I.M.S. Celebrated the Anniversary of its Foundation under the Patronage of the President Aoun. Hasbani: My priorities are to Support Medical Conferences and Medical Ethics
- A Team from MOPH in Wadi Khaled: It is not "Aleppo Button" but Skin Diseases Caused by Poor Hygiene
- Hasbani Receives a Delegation of the Orthodox Societies
- Issuance of a New Drugs Public Price List No. 17/2/28755 Date 2/8/2017
- Inauguration of the Diagnostic Services Division at Al-Makassed Philanthropic Islamic Association Hospital
- A Saudi Donation Granted to "Al-Makassed" Philanthropic Association under the Patronage of Hasbani
- Issuance of a New Drugs Public Price List No. 17/2/26706 Date 28/7/2017
- Hasbani Closed his Tour in West Beqaa with a Visit to Rachaya Hospital: the Influx of Migrants Prompted us to Develop a Strategy for Lebanon and the Health Sector in it
- Referral of The Director of Kherbet Kanafar Governmental Hospital to the Public Prosecution and Formation of a New Hospital Management Committee
- Hasbani Visited Amik, Kherbet Kanafar and Mashghara: West Beqaa is at the Heart of Governance Policies and Should be Supported to Keep People in their Country
- Issuance of a New Drugs Recalls Resolutions No. 1305/1 and No. 1306/1 Date 15/7/2017
- Hasbani Started his Tour in Beqaa with a Visit to Al-Azhar: I will Listen to the Concerns of People and Institutions on the Ground
- Issuance of a New Food Safety List No. 110
- Hasbani Received an in-Kind Saudi Arabia's Donation for the Health Sector and Opened a Dialysis Unit at Hariri University Hospital: the Continuing Support Enhances Humanitarian and Social Capacities
- About
- Hasbani Launched the 2025 Strategy during Beirut Healthcare Industry Forum: Towards a Paradigm Shift for Health Sector in Lebanon
- The Launch of Michael Haddad's Expedition to the North Pole to Raise Awareness about Climate Issues
- Hasbani Presented the Health Sector Strategy "Health 2025": "Achieving a Qualitative Leap in Ensuring Comprehensive Health Coverage and Maintaining the Dignity of the Citizen
- In the Presence of more than 500 Participants, Deputy Prime Minister Health Minister Inaugurates Beirut International Healthcare Industry Forum and Launches the Universal Healthcare Coverage for each Citizen. Hasbani: Lebanon has Sufficient Capacities to Attract investments into Health sector
- A $150 Million Package to Promote Health Care in Lebanon is Coming to Light
- Hasbani and his Egyptian Counterpart Finalized the Final Version of a Cooperation Agreement within the Scope of Health and Medicine
- Hospital mortality surveillance
- Minister Hasbani Launches the Healthcare Sector Strategy in Lebanon Monday July 10 in "Beirut International Healthcare Industry Forum"
- Hasbani Received from Antoinette Chahine her Book Entitled: "My Crime is that I was Innocent"
- Hasbani Representing the President of the Lebanese Republic in the Health Economic Forum for Arab Hospitals Federation: We are Working to Adopt Policies that Meet the Needs of Citizens and Regulate Health Expenditure
- The President of the Lebanese Order of Physicians Received the Initial Report on the Death of Kassab and Reported it to Hasbani
- Issuance of a New Drugs Public Price List No. 17/2/24320 Date 6/7/2017
- In-kind Saudi Arabian Aids Granted to Primary Health Care Centers and Governmental Hospitals and the Establishment of a Health Center in Beirut. Hasbani: A Step to Translate Special Relationships with Saudi Arabia and its Determination to always Stand with Lebanon
- Hasbani Refers the Board of Directors of Al-Bouar Governmental Hospital to the Central Inspection Authority
- Hasbani Issues a Decision to Continue the Board of Directors of Al-Bouar Hospital until the Formation of a New Board of Directors by the Council of Ministers
- Press Release on 19/06/2017 Concerning the Diagnosis of Infection with the MERS Coronavirus
- Press Release Issued by the Media Office of the Minister of Health Concerning the Attack on Bhannes Hospital
- Hasbani Sponsors the Launch of iBloodlink Application: A National Plan for Donation and the Ministry’s Doors are Open to Innovators
- Hasbani Visited Frangieh: We are Open for the Best of the Country
- Hasbani Honored from Moawad in Ehden: Our Participation in this Covenant is to Rebuild the Institutions
- Vector-Borne Diseases
- Hasbani Confirmed the Support for Governmental Hospitals by Investing in their Infrastructure . Hasbani in the Ceremony of Receiving Donation from the Italian Agency to Hariri Hospital: We are Proud of this Humanitarian Edifice that Provides Services to all Residents in Lebanese Territory
- A $ 150 million package to promote health care in Lebanon is coming to light
- A $ 150 million package to promote health care in Lebanon is coming to light
- Recruitment criteria for professionals working in mental health in humanitarian settings
- Guidelines and standards
- What Parents Need to Know about their Children
- MOPH Participation in the 70th World Health Assembly in Geneva
- Cornerstone Laid for the extension of Dar Al-Shifa Hospital in Abi Samra
- Press Release Concerning Organes Donation
- MoPH Closes the "Specialized Clinics Center" in Bhennin and Seizes 600 Types of Smuggled Syrian Medicines
- Hasbani: We Have Set up a Scientific Mechanism for the Financial Ceilings of Hospitals
- Hasbani: Let's keep the Health Sector and Financial Ceilings Away from Cheap Pricing and Politicization
- Hasbani Closed the Meetings of Services Coordination: We will Draw up Schedules for Big and Basic Projects
- Issuance of a New Drugs Public Price List No. 17/2/20709 Date 16/6/2017
- Laboratory Technician Exam
- Hasbani: There is an Attempt to Streamline Capitalism so as to Become a Free Economic System with Social Responsibility
- MoPH Closes a Clinic of Two Non-Lebanese Doctors in Choueifat and Refers Two Pharmacists to the Inspection
- Hasbani Follows up the Death of Farah Kassab and Issues Two Decisions and Two Letters to the General Prosecution and the Order of Physicians
- Accreditation Results 2014
- Hasbani Issued a Decision on the Regulation of Surgical Operations in Specialized Hospitals and Reminded Beauty Centers of the Legal Deadline Given until August to Settle their Situation
- Ministry of Public Health Closes the Doors of a Syrian Dietitian Center in Hamra with Red Wax
- MOPH is Investigating the Death of a Young Woman who was Transferred from a Beauty Hospital to “Our Lady of Lebanon” Hospital
- For your Health... Quit Smoking Now!
- Health Beyond Politics-2009
- Hasbani Announced the Japanese Aid for the Medical Equipments to Governmental Hospitals: We are Working on Developing the Performance of these Hospitals and their Infrastructure
- Hasbani Concluded his Southern Tour with a Visit to "Medrar" Association and Nabih Berri Governmental Hospital in Nabatieh: We are Proud of the Capabilities of our Health Sector in Lebanon and the Arab Countries
- Hasbani Visited the Governmental and Turkish Hospitals with Seniora and Bahia Hariri during his Visit to Saida: We are Approaching Practical Solutions to the Electoral Law
- Issuance of a New Drugs Public Price List No. 17/2/18843 Date 20/5/2017
- Back to his School, Hasbani Stressed the Importance of Audacity with Confidence and Courage. Hasbani to the Students of Beirut Annunciation Orthodox College: "Don't Be Afraid of Failure. Failure is the Key to Success."
- Office of Health Minister: Be Careful not to Spread any Case through the Media without Checking the Accuracy of the Information
- Issuance of the Food Safety List No.109
- Hasbani Participated in the World Economic Forum Held at the Dead Sea Hasbani: The Most Suitable Option is to Have a Governance Model which Based on the Economic Freedom Related to Social Responsibility
- A Canadian Delegation from the "International Accreditation Foundation" in a tour in the Primary Health Care Centers in Lebanon
- Stay Healthy this Summer
- Health Insight 2017 Forum
- Announcing "Beirut International Healthcare Industry Forum" to Be Held in July Hasbani: Lebanon's Position as a Destination for Medical Tourism will Be Enhanced and the Investment in this Sector will be Encouraged
- Hasbani: We will Launch a New Mobile Application that Facilitates Citizens' Admission to Hospital
- Hasbani Examined Drug Factories in Jadra, Chouwaifat and Jamhour: These Factories have Proved Successful and We are Working to Register the Lebanese Drug in the Foreign Markets.
- Issuance of a New Drugs Public Price List No. 17/2/16754 Date 16/5/2017
- During his Participation in the Arab Week for Sustainable Development in Cairo, Hasbani: Universal Health Coverage Plays a Crucial Role in the Achievement of Sustainable Development and the Reduction of Poverty
- Al-Bukhari Offers to Hasbani the Shield of Saudi Arabia's Foreign Affairs Ministry
- Minister Ghassan Hasbani Launching The National Nursing Capacity Building Project & Practiced Nursing for an Hour
- Hasbani Discussed with his Egyptian Counterpart the Declaration of Intent for Collaboration on Drugs between Egypt and Lebanon
- Issuance of a New Drugs Recalls Resolutions No.787/1 Date 13/5/2017
- Issuance of a New Drugs Recalls Resolutions No.733/1 Date 4/5/2017
- Hasbani Opened the Forum of Medical Tourism in the Presence of Minister of Tourism to Rectify the Wrong Viewpoint of the Medical Sector
- Hasbani Chaired a Workshop to Enhance Partnership between MoPH and the Media and Stressed the Importance of Primary Health Care Centers
- Hasbani during the Lunch of Zahleh –Based Lebanese Forces’ Coordinating Body: Outlawed Weapons Kill not only Citizens, but also Lebanon’s Image
- Hasbani Met Zahleh Deputies Bloc: We are Keen on the Cabinet’s Cohesion and what Happened Regarding the Electricity File has Nothing to do with Policy. We are Working to Achieve a Comprehensive Health Strategy
- Issuance of the Food Safety List No.108
- Hasbani Heading a Meeting For the Coordination & Cooperation Committee of the Public Funds Bodies
- Issuance of a New Drugs Recalls Resolutions No.690/1 Date 2/5/2017
- Issuance of a New Memo No.34 Date 4 May 2017 Concerning the Code of Ethics
- Issuance of the Lebanese Guidelines For Erythropoiesis-Stimulating Agents (ESAs) Approval in Non-Dialysis Chronic Kidney Disease (ND-CKD) Patients aT the MOPH
- Non Communicable Diseases Prevention and Control Plan (NCD-PCP) Lebanon 2016-2020
- Hasbani Visited Hariri at the Serail as He Follows up Electricity File: We Have Alternatives that Can Be Incorporated in the Terms and Conditions Book
- Hasbani Continues his Meetings at the World Bank and Succeeds in Securing $150 Million in Funding for the Lebanese Health Sector
- The First Tour Ever Undertaken by a Lebanese Health Minister to Pharmaceutical Factories. Hasbani: We are a Guarantor of Lebanese Drugs Quality
- Hasbani Begins his Tour of Drug Factories: We are Working to Raise the Industry's Level and Performance to Reach International Markets
- Lecture by Dr. Fadia Elias at NIH / NCI - Washington USA
- Hasbani: Register your Children and Keep your Nationality, Lebanon Needs your Energy
- Hasbani from Washington: There is a New Dynamic in the American Administration and a Significant Positive Attitude Towards Lebanon
- Hasbani Begins his Meetings in World Bank in Washington
- New Release of Good Laboratory Practices Guidelines for Pharmaceutical Quality Control Laboratories in Lebanon- 2017
- The Team of the Ministry of Health Completes its Investigations into the Death of a Syrian and Injuring his Relatives with Health Effects
- Media Centre
- Health Minister Visited PHC Centers in Beirut
- National Mental Health Campaign 2017
- Health Minister Visited PHC Centers and Hospitals in Beirut
- Launching of the National Mental Health Campaign 2017 in the Occasion of "World Health Day"
- Accreditation
- The National Mental Health Campaigns
- Hasbani: We are Seriously Considering the Organization of the Public Funds and the Standardization of their Health Related Provisions
- During a Discussion with Antonine School's Students, Hasbani: Food Safety is an Integrated Cycle and it is at the Core of the Ministry's Work
- Hasbani Chaired the Meeting of the Technical Committee for the Coordination of Baalbeck-Hermel Mohafaza
- Hasbani Chaired the Meeting of the Technical Committee for the Coordination of Keserwan District Services
- Hasbani from Bkerki: To Put the Electoral Law on the Cabinet Table as soon as Possible
- Closure of "Salam Khamsa" Slaughterhouse in Choueifat with Red Wax upon the Request of MOPH
- Press Release Concerning the Food Poisoning at Sagesse High School
- Minister Hasbani Inaugurates Lebanon HR Summit Conference Organized by CAREERS
- New Decision No.344 Date 29 March 2017 about the Updated Guidelines for the Drug Technical File Submission
- Mental Health and Psychosocial Support Task Force
- Press Conference to Raise National Awareness on Epilepsy
- A Letter from Hasbani to the Minister of Agriculture to Restrict the Importation of Brazilian Meats
- Press Release Concerning the Citizen Awatef Ghannoum
- Launching of the Strategic Plan for the Elimination of Tuberculosis in Lebanon
- Hasbani in an Interview with "NBN": The Expenditure of MOPH Amounts to Almost 600 Billion
- Hasbani Attended a Surgery for the Treatment of Epilepsy during which a Developed Device was Installed
- National Guidelines for Tuberculosis Prevention, Care and Elimination in Lebanon- 2017
- Vaccination Activities in Tripoli
- Minister Hasbani's Statement During his Visit to Tripoli
- Explaining the Case of "NSSF" Patient on "Al Jadeed" Hasbani: The Unification of the Public Funds is a Reform Step
- World Kidney Day 2016
- National Campaign for the Prevention of Obesity and Kidney Diseases 2017
- National Campaign for Cardiovascular Disease Prevention 2016
- National Campaign to Prevent Birth Defects among Newborns 2017
- National Campaign for The Prevention of Kidney Diseases and Obesity
- Randa Hamadé, passionnée, infatigable, inlassablement dévouée au service de la santé au Liban
- Minister Ghassan Hasbani: We Will Bring back Lebanon's Role as a Health Platform for Hospitalization in the Arab Region
- Minister Hasbani to "Al Jadeed" : The Budget is Meaningless Without Reforms
- Signature of a Partnership Agreement between Physiotherapists in Lebanon and France under the Auspices of the Minister of Public Health
- Hasbani in a Fundraising Event for Multiple Sclerosis: "We are Working to Ensure a Financial Sustainability to Prevent the Interruption of Chronic Disease Medicines"
- B-Population Data
- Hasbani: "53% of the Lebanese Patients are Treated at MOPH Expenses and We are Working on Improving the Hospitals Admission System"
- Hasbany Discussed with UNRWA the Health Status of the Palestinians and Asked Them to Ensure the Continuity of its Work to Spare the Lebanese Treasury from Additional Burdens.
- National Campaign to Prevent Birth Defects among Newborns
- Hasbani from Cairo: "To Unify the Standards of Medicines Exchange between the Arab Countries"
- Immunization Campaign Results (2014-2016)
- Timings of meetings
- Launching of the Vaccination Campaign under the Patronage of Prime Minister Hariri and Minister Hasbani
- Health Response Strategy - A New Approach 2016 & Beyond
- hasbany-discussed-with-unrwa-the-health-status-of-the-palestinians-
- Awards Gained
- 2 Hasbany Discussed with UNRWA the Health Status of the Palestinians and asked Her to ensure the Continuity of its Work to Spare the Lebanese Treasury from Additional Burdens
- Strategic Plan of the Ministry of Public Health 2016-2020 (Final Draft)
- Latest News concerning AH1N1 Flu
- Launching of the National Breastfeeding Campaign 2016
- Hasbani in a Dinner for Hemophilia Awareness:" We are Working to Raise Awareness to Promote Early Detection and Encourage Treatment Adherence"
- The Lebanese State Gives Priority to the Lebanese. Hasbani: "UNRWA Must Assume its Responsibility"
- Press Release Concerning the One Stop Shop for Administrative Services
- Minister Hasbani Allowed Pharmacists to Opt for Local Generic Medicines
- Press Release Concerning the Pharmaceutical Products GSDP Certificates Awarding Ceremony
- For the 1st Time Minister Hasbani Visits Koura Hospitals
- Hasbani:"If We Fail to Control Statements to Spare Lebanon from Negativism We Won't Be Able to Achieve the Economic Development"
- Visit of HE Minister Hasbani to Balamand
- Releasing the New Version of the Guidelines for Good Storage and Distribution Practices of Pharmaceutical Products in Lebanon
- Hasbani, French Counterpart Signed Cooperation Protocol: "We Work to Improve Quality of Serving Patients"
- The Cleft Lip National Awareness Campaign 2016
- Hasbani Visiting the "Smart Pharmacy" at "Mohammed Bin Rashid" Hospital in Dubai
- Hasbani: “Lebanon Provides High Quality Touristic and Hospitalization Services”
- Hasbani after Meeting Metropolitan Audi:"No Significant Differences in Principles and Aspirations on the Electoral Law"
- Hasbani: We Seek to Build a Modern State for the Future ... and We Will Launch the One Stop Shop Next Week
- Meeting between Minister Hasbani, OMSAR Team and the Syndicate of Restaurants
- Health System Resilience in Lebanon: A Consistent Progress amidst Political Instability
- Meetings of Minister Ghassan Hasbani at MOPH
- Lebanon Comes ahead of the Arab and Foreign Countries in Health Care
- Hasbani Participated in Arab Health Exhibition in Dubai
- National Tuberculosis Awareness Campaign 2016
- National Awareness Campaign on Organ Donation 2016
- A Delegation from MOPH Participated in the 45th Session of the Council of Arab Health Ministers in Cairo
- Communicable Diseases
- Meeting with Minister Hasbani Concerning "Al Bouar" Governmental Hospital
- Launching of the Cleft Lip National Awareness Campaign
- Meeting between Minister Ghassan Hasbani and the Governor of Beirut
- Launching of the Special Stamp of Poliomyelitis
- Press Release Issued by the Media Office of the Minister of Health
- National Awareness Campaign on Hemophilia 2017
- Launching of the National Awareness Campaign on Hemophilia 2017
- Minister of Health Visits Victims of the Terrorist Attack in Istanbul
- Press Release Concerning the Case of the Child Menissa Hasan
- Interview of Minister Ghassan Hasbani with "RLL"
- Press Release Concerning the Case of the Child Mohamad Barakat
- Meeting between Minister Hasbani, the Syndicate of Hospitals and the Red Cross: Concerning Patients Admissions to Hospitals
- Financial Burden of Cancer Drug Treatment in Lebanon
- Health System Resilience: Lebanon and the Syrian Refugee Crisis
- Health System Resilience: Lebanon and the Syrian Refugee Crisis
- Hand-Over Between the Health Minister Wael Abou Faour And The Current Minister Ghassan Hasbani
- National Competitive Bidding for Emergency Primary Healthcare Restoration Project EPHRP– Ref.: P152646
- Memorandum of Understanding between MOPH and MSF for the Rehabilitation of "Bar Elias" Hospital
- Christmas Tree Lighting Ceremony in Beit Lahya
- Press Release for the World Aids Day 2016
- Press Release about the Launching of the Maternal Mortality National Report- A Success Story in Lebanon
- Terms of Reference
- Photos of Accreditation Phase 4 Training Workshop (March 2015)
- Photos of PHC Accreditation Phase 4 Workshop (May 2015)
- Photos of Surveying Visits to PHC Centers within Phase 4 Accreditation Program
- Launching of Project
- Photos of Project Workshops
- Training Workshop on Simplification of Administrative Procedures for MOPH Staff
- C-MOPH Services Utilization Data
- H-Performance Contracting
- Acknowledgments
- Ethics of the Pharmacy Profession
- F-Diseases’ Surveillance Data
- Guidance and List of Requirements for Registration of Biosimilars Products
- Pharmaceuticals
- I-National Health Accounts
- G-Maternal Neonatal Mortality Notification System (MNMNS)
- Events & Conferences
- E-Vaccination and Campaigns
- D-Epidemiology
- B-Population Data
- A-Summary Tables
- Table of Contents
- Foreword
- Accreditation of Hospitals in Lebanon
- Accreditation Results 2006
- Accreditation Results 2005
- National Hospital Survey
- Marketing Lebanese Hospitals
- History
- Forward
- Hospital Accreditation
- Mop-Up Campaigns at Informal Tented Settlements during March & April 2015
- Immunization at Border Check Points (2015)
- Recreation Day at Ch'him
- Recreation Day at Riyadi Sports Club
- Recreation Days Held during Second National Polio Immunization Campaigns (2014)
- Cold Chain Training Initiative
- Educational Sessions Held at Tannourine (27th April 2015)
- Educational Sessions Held at Jbeil (28th April 2015)
- Educational Sessions Held at Akkar (29th April 2015)
- Vaccination at Jbeil (28th April 2015)
- Vaccination at Akkar (29th April 2015)
- World Immunization Week Activities (April, 2015)
- Laws & Regulations
- Mop-Up Polio Campaign (January and February 2016)
- Expanded Program on Immunization
- Laws and Regulations
- Training on PPD Test and Effective Management of Vaccines
- Training Workshop for Nurses with Order of Nurses in Lebanon
- Training on Use and Distribution of Cholesterol & Triglyceride Machine
- Training on Use & Distribution of HbA1c
- Launching of Breast Cancer Awareness Campaign 2016
- The 13th Lebanese Society of Medical Oncology (LSMO) National Forum
- Lauching of World Health Day 2016
- Launching of World Kidney Day 2016
- Launching of the New Birth Registry
- Launching of the Universal Primary Care Towards Universal Health Coverage Project at the Grand Serail
- World Health Day 2013
- Announcement of the Results of the Grading System for Restaurants
- World AIDS Day 2015
- The Palliative Care International Day
- Conference on Mother & Child Health Program
- Launching of The Vaccination Campaign Against Polio 2013
- Launching of the World Diabetes Day 2013
- ESA Workshop on Projects Undertaken by MOPH with the Support of the French Ministry of Social Affairs and Health
- Participation of the Ministry of Public Health in Health Insight 4 Conference.
- Launching of Breast Cancer Awareness Campaign 2015
- Launching of Breast Cancer Awareness Campaign 2014
- Launching of Breast Cancer Awareness Campaign 2013
- Launching of Breast Cancer Awareness Campaign 2012
- Breast Cancer Awarness Campaign 2014
- National Blood Donation Campaign 2016
- National Breastfeeding Campaign 2016
- Breast Cancer Awareness Campaign 2016
- Summer Health Tips
- Sun Exposure Health Tips
- Breastfeeding Tips
- Best Nutrition Advice for School-Aged Children
- Call for Research Proposals: Research in Priority Areas of Public Health 2016–2017
- Job Opportunities Announcement
- Competency Test to Practice the Profession of Medical Laboratory Technology (BS Level)
- Postponement of Health Inspectors Exam
- Health Inspectors Exam
- Clarifiation About (AH1N1)
- Press Release Concerning the Prevention of H1N1 Flu
- Press Release Concerning Zika Virus
- Press Release Concerning a Death Caused By Malaria
- Press Release Concerning the Meningitis Case in Akkar
- Press Release Concerning the Spread of Mosquitoes in some Areas in Lebanon
- Press Release Concerning H5N1 Bird Flu in Nabi Sheet
- Press Release Concerning Hepatitis A
- New Report Issued by MOPH about the Actions Taken Concerning Hepatitis A
- New Report Issued by MOPH Concerning the Actions Taken about the Hepatitis A
- Cornerstone Laid for the New Service of Public Health in the Western Bekaa
- MOPH Announces Alert Against the Sandstorm
- Press Release Concerning AH1N1
- Warning of the Ministry of Public Health about Thallium
- Leishmaniasis
- Job Opportunities
- MOPH Strategic Plan 2007-2012
- Health Reform in Lebanon
- Ministry of Public Health Strategy Orientations
- Cornerstone Laid for the New Building of Beirut Karantina Governmental hospital
- New Decision Issued Nb. 1292 Date 10/10/2016 Concerning the Update of the OTC
- Draft “Inter-Ministerial Substance Use Response Strategy for Lebanon 2016-2021” for Public Review
- Lebanon Ranked 34 in Health with a Score of 6.8 out of a Total of 7 in the Global Competitive Report 2016-2017
- Launching of the National Guidelines for the Medical Implants
- Award of the Dr A.T. Shousha Foundation Prize and Fellowship
- Award of the Dr A.T. Shousha Foundation Prize and Fellowship
- Referral of Afif Hammoud to the Public Prosecution Discriminatory
- Training Workshop on Simplification of Administrative Procedures
- Japanese Donation for Improving the Health Care of Chronic Diseases under the Patronage of HE Minister Abou Faour
- YouTube Channel
- ”Full Hospitalization Coverage for Elderly“ by Dr Walid Ammar on Alam Al Sabah Show
- Inauguration of the Department of Gynecology and Obstetrics in Baabda Governmental Hospital
- Opening of Free Radiotherapy Treatment Center for Cancer Patients Covered by MOPH
- Opening of free Radiotherapy Treatment Center for Cancer Patients Covered by MOPH
- Opening of free Radiotherapy Treatment Center for Cancer Patients Covered by MOPH
- Opening of free Radiotherapy Treatment Center for Cancer Patients Covered by MOPH
- Draft “Inter-Ministerial Substance Use Response Strategy for Lebanon 2016-2021” for Public Review
- Draft “Inter-Ministerial Substance Use Response Strategy for Lebanon 2016-2021” for Public Review
- Meeting between Abou Faour and the Syndicate of Hospitals Concerning the Full Hospitalization Coverage for the Elderly
- Announcement of the Results of the Grading System for Restaurants in Kesrwan
- Syrian Refugees Crisis Impact on Lebanese Public Hospitals- Financial Impact Analysis: APIS Report
- GSDP Facility Questionnaire Edition 2
- Minister Abou Faour Acknowledged the NSSF and Minister Azzi the Full Coverage of the Expensive and Cancer Drugs
- Closure of "Beirut Beauty Clinic Center"
- Referral to the Public Prosecution of 5 Sports Clubs
- Abou Faour Announced the Full Coverage of the Expensive and Cancer Drugs by the Cooperative of Government Employees
- Referral of a Complaint against a Dispensary to the Ministry of Social Affairs
- Closure of the Specialized Clinics Center in Akkar
- Announcement of the Start of Full Hospitalization Coverage for the Elderly Next Month
- Training for the Radiologists and Nurses as Part of the National Breast Cancer Awareness Campaign
- Referral to the Public Prosecution Mr. Moussa Pretending to be a Health Inspector
- Abou Faour Visiting the Lebanese University in Rachaya
- Health Tips
- Summer Health Tips
- A Certificate of Appreciation to MOPH at the Food Safety Conference in Oman
- Launching of the National Campaign for Cardiovascular Disease Prevention
- Launching of the Code of Ethics for Medicinal Products Promotion in Lebanon and Implementation Procedures at the Grand Serail
- Best Nutrition Advice for School-Aged Children
- Prohibition of Selling some Pharmaceuticals Products without Medical Prescription
- MOPH Reduced the Public Pricing of Generic Drugs
- Recalls of Medical Devices from the Lebanese Market
- Launching of the MOPH Campaign in Collaboration with the Unicef & "Beyond"Organization to Reach 1200 Syrian Settlements
- New Release of the Lebanon National Drug Index- Fifth Edition
- Products Recalls From the Lebanese Market
- Referral of "Mectapharm" from MOPH to the Public Prosecution
- Minister Abou Faour Open an Investigation into the Cause of the Death of the Child Elio Salloum in Ajaltoun
- Referral of "Belle vue Medical Center Hospital" and "Avent" Company from MOPH to the Public Prosecution Discriminatory
- Prohibition of Selling the Medical Product Ethyl Chloride Without Medical Prescription
- Press Release Concerning the Repercussions of the Sandstorm
- Closure of "K & A- Machmouchi" Pharmacy in Dbayeh
- Ministry of Health Disseminates New Procedure to Follow up Citizens’ Complaints
- Recalls of Medical Devices Produced by Silimed Company- Brazil
- Closure of "Health Clinics" in Ashrafieh
- New Decision No.224 Date:19-2-2016 Concerning Drugs Recalls from the Lebanese Market
- Minsiter Abou Faour Asked Minister Hajj Hassan to Ensure the Safety of Salt Production Procedures
- Closure of "MaM'S Hug" Nursery in Khalde
- Closure of Two Non-licensed Nurseries "La Pepiniere " in Clemenceau and "ElJoudi" in Hadath
- Closure of "Petit Monde" Nursery
- Referral of the "Foodwatch" Organization Scientific Report Concerning "Kinder" Products to the Ministry of Economy and Trade
- Press Conference for Minister Abou Faour in the World Day of Viral Hepatitis
- Closure of Dr. Imad Al Zuhairi Clinic in Chiyah
- EU/IfS Project
- Short-Term Hospitals Accreditation
- MOPH Participation in the 68th World Health Assembly in Geneva
- Minister Abou Faour Instructed the Staff of Drugs Committee to Receive Drugs Application Only from the Patient or One of his Relatives
- Minister Abou Faour:" Assigning Priority to the Local Drug Manufacturing Industries Will Lead in Reduction of Drug Prices."
- Closure of 6 Non Licensed Nurseries
- Warning from MOPH to Rim Water Company in Antelias
- Closure of two Pharmacies and Referral of one Illegal Pharmacy to the Public Prosecution Discriminatory
- Closure of "Fimalco" Warehouse and Request from HE Minister of Interior Closure of "Dental World" Company
- Minister Abou Faour Announces the Immediate Closure of any Institution Violating the Required Health Conditions
- Minister Abou Faour Asked the Ministers of Defense and Interior to Control the Trucks Carrying Chicken Guts to Feed the Fish in "Al Assi"
- The Ministry of Public Health Opened an Investigation about Poisoning Cases in Iklim AlKharoub
- Meeting between Minister Abou Faour and Professor Chebel Mourani President of Association of Children with Kidney Disease
- Prohibition the Entry of Some People to MOPH Offices
- MOPH Transferred the Governmental Hospitals Dues to the Ministry of Finance
- Press Conference for Minister Abou Faour after his Meeting with the Governmental Hospitals
- Signature of the Contracts Related to "Sheikh Khalifa Bin Zayed Al Nahyan " Hospital by Minister Abou Faour and UAE Ambassador
- Prohibition the Entry of Rida Hachem to MOPH Offices
- Health Inspectors Exam on 8/10/2016
- Press Conference for HE Minister Abou Faour
- Minister Abou Faour Decided to Withdraw the Medical License of Dr. Alam and to Close his Clinic
- Joint Meeting Between Ministers of Health, Economy and Agriculture to Follow up on Wheat Safety
- Press Conference for HE Minister Abou Faour and Miss Lebanon Concerning Health Care Benefits to Mothers & Children
- Detection of Fraud in "Al Assi" Hospital and Referral of files to Public Funds
- An Agreement with the Ministry of Labor to Expand the Coverage to 100% for Expensive Drugs
- New Agreement with the Lebanese University to Establish the National Center For Drugs Quality
- Minister Abou Faour Inaugurated a Primary Health Care Center in Rafic Hariri Hospital
- Closure of "Kids Care" Nursery in Tripoli
- Meeting Between HE Minister Abou Faour and President of the Order of Physicians Professor Boustani
- Report of the National Emergency Committee in Charge of the Health Risks Assessment of Waste Crisis and Propose Solutions
- Emergency Committee to Evaluate Trash Crisis Risks
- Minister Abou Faour Suspends the Contract with "Sacré Coeur" Hospital
- HE Minister Abou Faour Decided to Re-Open the Universal Hospital
- New Resolution Concerning the Good Storage & Distribution Practices (GSDP) for Pharmaceutical Products
- Warning from MOPH to "The National Distribution Company"
- Minister Abou Faour Ordered to Stop Working in Samih al Natour's Establishment
- Minister Abou Faour Referred Doctor Sabbagh to the Order of Physicians of Beirut
- Press Conference for HE Minister Abou Faour on 30-9-2015
- Health System Resilience Amidst Political Instability: the Case of Lebanon
- Minister Abou Faour Visit to Judge Ali Ibrahim
- Minister Abou Faour Referred to the Financial Public Prosecutor 9 Controller Doctors
- Meeting at MOPH Concerning the Unified Medical Prescription
- Meeting with HE Minister Abou Faour Concerning Batroun Hospital
- Meeting Between HE Minister Abou Faour and the Medical Errors Committee
- HE Minister Abou Faour Decided to Close Siham Itani Pharmacy in Beirut
- Minister Abou Faour Cancel the Contract with "El Salam" Hospital in Tripoli
- Meeting at MOPH to Follow up the Side Effects of the Sandstorm
- HE Minister Abou Faour Conducted Final Discussions Concerning The Unified Prescription Form
- Recruitment of Quality Auditors for Good Storage & Distribution Practices (GSDP)
- Guides for the Drug Technical File Submission: Module 3 (S and P Parts) and Module 5 (Bioequivalence Study)
- Temporary Closure of " Universal Hospital"
- Press Conference for HE Minister Abou Faour on 3-8-2015
- Reminder from MOPH: The Unified Prescription Form will be Effective as of August 10,2015
- MOPH to Investigate Body Found in Saida Governmental Hospital Bathroom
- Minister Abou Faour Decided to Withdraw the Licence of two Medical Doctors
- Press Conference for HE Minister Abou Faour on 27-7-2015
- Press Release on 15-9-2015 Concerning the Garbage Crisis
- MOPH Recovered from Hospitals Sums of Money Related to False Bills
- Referral of the Food Poisoning File to the Public Prosecution Discriminatory
- Invitation for Launching the Management & Health Standards for Child Safety & Protection in Nursery
- MOPH Launched the Revised Version of the Service Delivery Guidelines of Reproductive Health
- Closure of the Medical Center "Dar El Wafa" in Dohat Aramoun
- Extension of the Deadline of Issuing Health Permits for Drinking Water Treatment Companies
- New Decision of HE to Prevent the Use of "Ain Bteghrin" Water
- Closure of a Dispensary and Issuance of a Warning to a Person Selling Drugs Illegally
- Press Conference for HE Minister Abou Faour on 19/5/2015
- Salary Domicilation of Governmental Hospitals Employees
- Referral of The Responsible of a Warehouse Containing Chemicals and Suspicious Medical Material to The Public Prosecution Discriminatory
- Warning from MOPH to Bottled Water Companies
- MOPH Referred a Citizen to the Public Prosecution Appeal
- Latest News Concerning Tuberculosis Cases
- Approval of the Final Version of The Unified Medical Prescription
- New Decision Concerning Closure of all Non-Licensed Nurseries
- Launching of Vaccination Campaign for Hepatitis "B"
- Closure of Nursery "Dima"
- Closure of Non Certified Beauty Center in the North
- Transfering an Amount of the Financial Ceiling of Private Hospitals in Akkar to Abdalla Elrassi Government's Hospital in Halba
- Reactivation of the Contract with Hotel Dieu Hospital
- Increasing the Number of Physicians of the Medical Committee of Beirut
- Open an Immediate Investigation into the Cause of the Death of the Child Abdel Raouf Elhouli
- Closing of the Minieh Hospital
- Minister Abou Faour Welcomed the Birth of Twin Boys
- Minister Abou Faour Suspends the Contract with Hotel Dieu Hospital
- Meeting at MOPH Concerning Unified Prescription Form
- Abou Faour Called the Order of Physicians for Immediate Printing of the Unified Medical Prescription
- Abou Faour Referred Medical Errors File to the Public Prosecution Discriminatory
- Patient Record Referral to the Public Prosecutor Discriminatory
- New Regulation Concerning the Importation of not Registered Drugs, Food Supplements & Energy Drinks
- MOPH is Following Up Amal Skaff's Case
- Dr Walid Ammar, the DG of Health is Participating in the 136th WHO Executive Board Session
- Press Release: WHO Mission to Lebanon to Assess the Country's Readiness for Ebola
- Minister Abou Faour Following Up on the Death of Miss Louisette Mansour with Concerned Hospitals
- Press Conference for HE Minister Abou Faour Concerning Wheat Safety
- World Health Day 2016
- Surveillance Data
- New Guidelines for Osteoporosis Assessment and Treatment
- National Cancer Registry
- New Guidelines for Osteoporosis Assessment and Treatment
- Osteoporosis Assessment and Treatment
- Referral of "Bay Rock" Restaurant to the Public Prosecution Appeal
- Press Conference for Minister Abou Faour Concerning the Improvement of Wheat Storage Conditions
- Launching of Hospitalization Coverage by 100% for Elderly
- Meeting between Minister Abou Faour and a Delegation of Wheat Farmers in the Bekaa
- Photos From Arsal ITSs (27th April 2015)
- Photos From Brital ITSs (24th March 2015)
- Photos From Hermel ITSs (24th March 2015)
- Photos From Akkar-Halba & Hayssa ITSs (23rd March 2015)
- Photos From Baalbek & Taybet Baalbek (23rd March 2015)
- Photos From West Bekaa- Joub Jannine, Kamed El-Laouz, Ghaze ITSs (23rd March 2015)
- Photos From Qobb Elias ITSs (23rd March 2015)
- Photos From South ITSs (23rd March 2015)
- Health System and Reform In Lebanon - 2003
- Referral to the Judges Hammoud and Ibrahim of Several Municipalities and Laboratories Disposing of their Wastes in the Litani River
- Ethics
- Press Release Concerning the State of Mauritania
Let us help you
Read about the latest topics.
Read about the latest topics.
Universal Health Coverage: Bridging the Gaps
Universal Health Coverage:
Bridging the Gaps [1]
Walid Ammar MD., Ph.D.[2]
Bridging the Gaps [1]
Walid Ammar MD., Ph.D.[2]
- Universal Health Coverage and the Lebanese Dilemma
Achieving Universal Health Coverage (UHC) is a main goal of the National Health Strategy, and is based on the principles of justice, equity, poverty reduction and the rational use of resources. It requires financing or providing preventive and curative quality health care for all, to satisfy each one’s needs against affordable contributions. Whereas alleviating the financial burden, as much as possible, on households, especially the poor, remains a main objective of UHC.
The purpose of Universal Health coverage is to ensure universal accessibility to services that address population health needs and country health priorities with adequate quality, without incurring households financial ruin. This implies reaching a consensus over two major policy decisions: 1st defining a benefit package, and 2nd, setting an acceptable level of financial burden on households, more specifically the OOP bearable level by income category. Starting up from scratch, the benefit package would include essential health services such as PHC, and the government would cover as much health interventions as its budget allows, by beginning with the most cost effective ones such as immunization, TB treatment and prenatal care. Thus the population would expect regular upgrading of the system and would welcome incorporating progressively more advanced services such as renal dialysis, treatment for cancer, and sophisticated surgeries. The dilemma of the health system in Lebanon is the current existence of a universal coverage for tertiary care and sophisticated treatments such as open heart and joint replacement surgeries and expensive cancer patent drugs, whereas, paradoxically, prevention and PHC services are not universally covered.
The purpose of Universal Health coverage is to ensure universal accessibility to services that address population health needs and country health priorities with adequate quality, without incurring households financial ruin. This implies reaching a consensus over two major policy decisions: 1st defining a benefit package, and 2nd, setting an acceptable level of financial burden on households, more specifically the OOP bearable level by income category. Starting up from scratch, the benefit package would include essential health services such as PHC, and the government would cover as much health interventions as its budget allows, by beginning with the most cost effective ones such as immunization, TB treatment and prenatal care. Thus the population would expect regular upgrading of the system and would welcome incorporating progressively more advanced services such as renal dialysis, treatment for cancer, and sophisticated surgeries. The dilemma of the health system in Lebanon is the current existence of a universal coverage for tertiary care and sophisticated treatments such as open heart and joint replacement surgeries and expensive cancer patent drugs, whereas, paradoxically, prevention and PHC services are not universally covered.
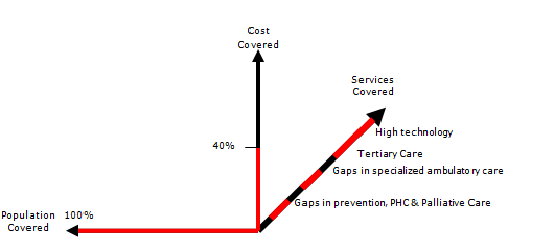
Therefore, while the population is looking up for more and more technologically advanced interventions, the public opinion would not be particularly enthusiastic about enhancing the coverage of essential services such as introducing new vaccines to the immunization calendar, mental health and safe motherhood care. Consequently, politicians would not venture a UHC plan that may disappoint their voters.
Nevertheless, technically, the main issue for achieving UHC in Lebanon remains the accessibility to a comprehensive package of PHC services including promotive, preventive and palliative care in addition to early diagnosis and early treatment.
- Scaling-up PHC and reducing OOP as a Strategic Direction
The 1998 National Health Accounts revealed that Total Health Expenditures (THE) represented 12.3% of GDP of which 60% were Out-Of-Pocket (OOP) payments. There is no doubt that oversupply in addition to focusing on financing curative care, and the poor quality of preventive and primary health care at that time, have contributed to over consumption of expensive diagnostics and treatments provided by the private for profit sector.
The MOPH historically covers In-patient services and expensive treatments. Ambulatory services were mostly uncovered, and therefore most OOP were spent on medication and outpatient services. The development of a wide network of PHC centers providing quality services that are accepted as an alternative for the private outpatient care, became the main goal of the MOPH to ensure universal accessibility to health care.
The success of the MOPH in decreasing the THE to 7.5% of the GDP in 2012 mainly by decreasing the OOP to reach 37% of THE, confirms the pertinence of reorienting its strategy towards PHC, especially that rationalization of households health expenditure was associated with an increased utilization of health services along with quality improvement. This was consolidated by a positive overall impact documented by a significant improvement in health indicators. Nevertheless, the OOP is still considered relatively high which requires moving further along the same strategic direction towards achieving UHC.
The MOPH historically covers In-patient services and expensive treatments. Ambulatory services were mostly uncovered, and therefore most OOP were spent on medication and outpatient services. The development of a wide network of PHC centers providing quality services that are accepted as an alternative for the private outpatient care, became the main goal of the MOPH to ensure universal accessibility to health care.
The success of the MOPH in decreasing the THE to 7.5% of the GDP in 2012 mainly by decreasing the OOP to reach 37% of THE, confirms the pertinence of reorienting its strategy towards PHC, especially that rationalization of households health expenditure was associated with an increased utilization of health services along with quality improvement. This was consolidated by a positive overall impact documented by a significant improvement in health indicators. Nevertheless, the OOP is still considered relatively high which requires moving further along the same strategic direction towards achieving UHC.
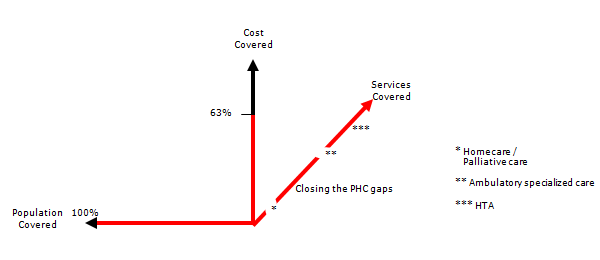
In addition a model for covering ambulatory specialized care in the public hospitals’ out-patient departments to fill this important gap in the current system, represent an affordable option assuming good adherence to the set rules, particularly the respect of the referral system by considering the PHC center as a gate keeper.
The cost born by the government for providing PHC and public secondary health services is equivalent to almost the third of the cost incurred by the individuals when purchasing themselves the services directly from the private sector.
In addition to the alleviation of the household financial burden by increasing government investment, part of direct disbursement upon utilization (OOP) could be shifted to a prepayment mode, through a community health insurance model. A World Bank financed project, designed to pilot this model by recruiting the extreme poor in a community “fidelity” scheme, is currently under implementation.
The cost born by the government for providing PHC and public secondary health services is equivalent to almost the third of the cost incurred by the individuals when purchasing themselves the services directly from the private sector.
In addition to the alleviation of the household financial burden by increasing government investment, part of direct disbursement upon utilization (OOP) could be shifted to a prepayment mode, through a community health insurance model. A World Bank financed project, designed to pilot this model by recruiting the extreme poor in a community “fidelity” scheme, is currently under implementation.
- The Cost of ensuring financial fairness through Universal Health Coverage
Calculating the cost of exempting the poorest and decreasing the contribution of the less poor, necessitates defining those categories and calculating their health spending. The current distribution of THE by source of health financing is as follows:
43% of THE are Out-of-pocket spending
27% of THE are General Government Spending. These include the totality of the MOPH budget, 25% of the NSSF spending, and health care budget items of the remaining public funds.
28% of THE are prepayments that include private insurance premiums and NSSF employees and employers contributions.
According to the Household Living Conditions Survey of 2004-2005, the OOP spending is distributed by income categories as follows: 30% paid by households with a monthly income lower than 650 thousand LBP; 30% by households earning between 650 thousand and 1,200,000; and finally the income category of more than 1,200,000, contribute the remaining 40% of the total OOP spending on health. Knowing that a significant proportion of the latest category spending is on supplementary and luxury goods and services like food supplements, cosmetics and plastic surgeries.
The target for achieving equity in health financing and alleviating poverty would be set as to achieve complete exemption of the poorest from any payment, and decrease the health spending of the less poor by half.
Considering that Total Health Expenditures (THE) represent around 7.41% of GDP and OOP spending 43% of THE, then OOP amounts to 3.19% of GDP. This is distributed over the three aggregated categories of income respectively 0.957%, 0.957%, 1.276%. Accordingly, the amount that needs to be alleviated from the households burdens amounts to 1.4355% of GDP (0.957%+0.957%/2).
If we consider the 2009 GDP of 53,000 Billion LBP; the estimated reduction of OOP would be around 760 Billion LBP. However, this does not mean that the cost incurred by the government needs to be as mush. From our experience, the cost born by the government for providing PHC and public secondary health services is equivalent to almost the third of the cost incurred by the individuals when purchasing themselves the services directly from the private sector. Accordingly, the estimated cost of the project would be around 250 Billion LBP which corresponds to increasing by 24% of total government spending on health in 2009. This estimate assumes good adherence to the set rules, particularly the respect of the referral system between the PHC centers and governmental hospitals, and the prescription of generic drugs. This might be ambitious to achieve in short term, nevertheless, the cost of the first stage of the project concerning the universal accessibility to essential services is perfectly affordable under current circumstances as shown in section VI.
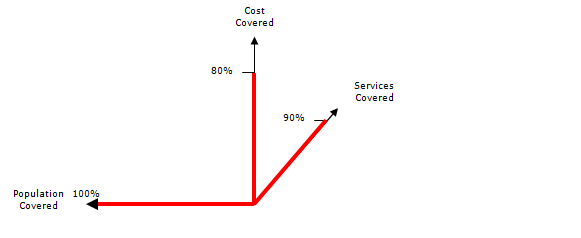
43% of THE are Out-of-pocket spending
27% of THE are General Government Spending. These include the totality of the MOPH budget, 25% of the NSSF spending, and health care budget items of the remaining public funds.
28% of THE are prepayments that include private insurance premiums and NSSF employees and employers contributions.
According to the Household Living Conditions Survey of 2004-2005, the OOP spending is distributed by income categories as follows: 30% paid by households with a monthly income lower than 650 thousand LBP; 30% by households earning between 650 thousand and 1,200,000; and finally the income category of more than 1,200,000, contribute the remaining 40% of the total OOP spending on health. Knowing that a significant proportion of the latest category spending is on supplementary and luxury goods and services like food supplements, cosmetics and plastic surgeries.
The target for achieving equity in health financing and alleviating poverty would be set as to achieve complete exemption of the poorest from any payment, and decrease the health spending of the less poor by half.
Considering that Total Health Expenditures (THE) represent around 7.41% of GDP and OOP spending 43% of THE, then OOP amounts to 3.19% of GDP. This is distributed over the three aggregated categories of income respectively 0.957%, 0.957%, 1.276%. Accordingly, the amount that needs to be alleviated from the households burdens amounts to 1.4355% of GDP (0.957%+0.957%/2).
If we consider the 2009 GDP of 53,000 Billion LBP; the estimated reduction of OOP would be around 760 Billion LBP. However, this does not mean that the cost incurred by the government needs to be as mush. From our experience, the cost born by the government for providing PHC and public secondary health services is equivalent to almost the third of the cost incurred by the individuals when purchasing themselves the services directly from the private sector. Accordingly, the estimated cost of the project would be around 250 Billion LBP which corresponds to increasing by 24% of total government spending on health in 2009. This estimate assumes good adherence to the set rules, particularly the respect of the referral system between the PHC centers and governmental hospitals, and the prescription of generic drugs. This might be ambitious to achieve in short term, nevertheless, the cost of the first stage of the project concerning the universal accessibility to essential services is perfectly affordable under current circumstances as shown in section VI.
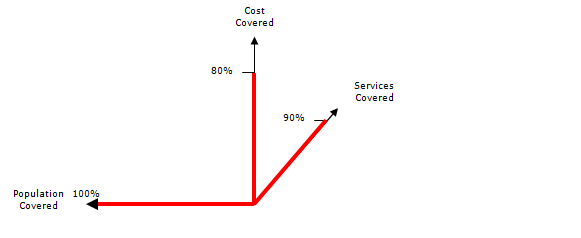
- Primary Health Care: The MOPH-NGOs-Municipalities partnership
Primary Health Care services have proved to achieve significant outcomes compared with the modest resources they need. In addition, the contractual relationship of the MOPH with NGOs have contributed to streamlining PHC services provided by NGOs and to rationalizing the spending through shifting more funds towards promotion and prevention. This relationship is based, on one hand on the centers’ commitment to improve the health status of the community by providing a comprehensive package of PHC services according to WHO’s definition; And, on the other hand, the MOPH provision of free-of-charge vaccines and essential drugs in addition to setting quality standards and clinical protocols, as well as ensuring the required training of NGOs Staff. What distinguishes this relationship is the MOPH in-kind contributions (replacing the conventional fee-for-service reimbursement), against centers' commitment to achieve better health outcomes. This mechanism avoids incentives for over consumption and encourage tailoring interventions according to community’s needs. This relationship constituted a more effective alternative compared to traditional financial subsidies provided by other Ministries to NGOs, whereby the government has not been able to control spending or even evaluate the results of its investment. By their nature, the MOPH contributions, whether related to its normative role or to the supply of vaccines and generic drugs, cannot serve but the intended purpose of the contract. On the other hand, the involvement of Municipalities as third parties enhances community participation in orienting, managing, and evaluating PHC services.
Strengthening the network of primary health care centers, and linking them to government hospitals through a referral system, is a key pillar of the national health strategy. This network is covering gradually all cities, neighborhoods and villages, benefiting from a geographic information system indicating the groups of habitats that are to be included.
Achieving Universal Health Coverage in Lebanon requires the adoption of government financing modalities linked to community enrollment of citizens providing them foremost access to preventive services, early diagnosis and early treatment, which will reflect positively, not only on the health status and budget of households, but also on public health and total health expenditure.
Strengthening the network of primary health care centers, and linking them to government hospitals through a referral system, is a key pillar of the national health strategy. This network is covering gradually all cities, neighborhoods and villages, benefiting from a geographic information system indicating the groups of habitats that are to be included.
Achieving Universal Health Coverage in Lebanon requires the adoption of government financing modalities linked to community enrollment of citizens providing them foremost access to preventive services, early diagnosis and early treatment, which will reflect positively, not only on the health status and budget of households, but also on public health and total health expenditure.
- Community health coverage to ensure universal accessibility to a basic benefit package
This is a decentralized coverage design consisting of the following:
- An essential basket of preventive and curative services will be available to all the population with no exceptions, and are provided through the network of PHC centers and governmental hospitals. The program targets primarily individuals not covered for ambulatory care by other insurance schemes.
- A catchment area for each health center within the national PHC network is defined, and the health center is connected to a governmental hospital through a referral system.
- A steering committee will be created in each catchment area to establish a community based enrollment system with representatives of the local authorities. The committee initiates activities to create awareness and attract people, especially the poor and the marginalized.
- Each beneficiary should first join one of the health centers chosen in his/her geographic area which will be his/her first point of contact with the health system. The Center will refer applicants to the designated governmental hospital in the area to complete their medical check up.
- The health center provides preventive and primary health care services including clinical and diagnostic tests for early detection of chronic diseases. Whenever the needed tests or treatment are not available at the health center, the patient is referred to the outpatient department in the district governmental hospital for investigation, treatment or hospitalization if needed.
- Referrals from the district governmental hospital to more specialized governmental hospitals, or to the central governmental university hospital in Beirut will be done when needed.
- Whenever the case cannot be treated in governmental hospitals, the patient will then be covered by the MOPH for treatment in a private hospital provided he/she follows the proper referral channels.
- Enrollment in the network and issuance of the health card will be for free for the poorest who will also benefit from co-payment exemption for needed services. The poorest will be identified by the Ministry of Social Affairs (MOSA) Poverty Targeting project. The MOSA will cover their health card fees and co-payment.
- The individual’s enrollment fee is determined so that the family’s annual contribution does not exceed a certain lump sum. Enrollment of those not identified by the poverty project requires buying the health card over two installments: The first paid to the public hospital, the second to the health center. Children and adolescents in the family receive the card for free.
- As soon as the first installment is settled, the insured will benefit from a free consultation and medical screening tests as appropriate to his gender and age, and the infants will get completely immunized as per the national immunization calendar. The Governmental hospital will establish an electronic medical record for each enrolled which will be electronically sent to the referring health center and the MOPH at the same time.
- The health center provides the MOPH with a list of all the enrollees, and the MOPH issues a membership card and establishes a unified database for all beneficiaries linked to health centers and governmental hospitals.
- The relationship between the MOPH and the NGO running the health center is governed by a contractual agreement which include the municipality as partner. The steering committee will make sure that services are provided to beneficiaries according to the contract. From its part, the municipality would contribute to the upgrading of the center’s services according to community needs.
- The MOPH provides financial support for each center according to the number of enrollees, in addition to providing essential drugs and vaccines (imported through the UNICEF) and drugs for chronic illnesses (purchased through the YMCA), as well as providing necessary training and technical support.
- The MOPH contracts with government hospitals to provide outpatient services not available in the health center such as specialized consultations, laboratory tests and diagnostic services, and covers the necessary costs.
- Drug prescriptions and tests will be administered according to well defined protocols. The MOPH will provide only generic medicines while health centers and governmental hospitals would adhere exclusively to the essential drugs list.
- This scheme does not cover neither consultations in private clinics and laboratory tests in private labs, nor drugs purchased from private pharmacies.
- Private insurance companies and mutual funds are allowed to collect the second installment of the health card and issue in return a complementary health insurance policy to those who choose to do so.
- Financing Model and Financial Implications
This is not a project for establishing a “health insurance” financing model funded by adherents’ contributions. Pooling risks through mandatory adherence is not considered as a requirement for two reasons: first, bad risks that incur expensive tertiary care are already covered by the MOPH for hospitalization and second, the Government decision is to allocate treasury funding for this kind of essential health services. This would rather be a voluntary enrollment system to constitute a catchment population that is loyal to a particular health center. The enrollment fee serves two objectives: first, it makes the NGO liable to the enrollee who in return would claim his rights to get the whole range of services included in the package, and second, to transform into prepayment some of the OOP spent on health care when purchasing the services, while reducing it significantly.
On the other hand, the enrollment would allow for a kind of capitation based financing where the MOPH links its payment to the number of enrollees avoiding thus inflationary fee for service reimbursement. This system would also incite the health center to provide quality services in order to attract enrollees and therefore generate more revenues and at the same time promote early diagnosis and rational follow up.
This program is expected to double the revenues of the health centers in the first year, enabling them to attract additional qualified human resources and enhancing their capability to providing quality services.
The increase in the activities of the centers will lead to increased demand for essential medicines provided or funded by the MOPH and will incur additional administrative burdens on the primary health care department, which will require additional human and financial resources. The expected cost of this initial phase is 60 Billion LBP from which the government will have to contribute with 40 Billion LBP representing only around 6% of the 2013 MOPH budget.
[1] This working paper elaborated in April 2014 was behind the development of the WB project on UHC that started implementation mid 2016.
[2] Director General of the Ministry of Public Health.
Professor at the Faculty of Medicine- Lebanese University
On the other hand, the enrollment would allow for a kind of capitation based financing where the MOPH links its payment to the number of enrollees avoiding thus inflationary fee for service reimbursement. This system would also incite the health center to provide quality services in order to attract enrollees and therefore generate more revenues and at the same time promote early diagnosis and rational follow up.
This program is expected to double the revenues of the health centers in the first year, enabling them to attract additional qualified human resources and enhancing their capability to providing quality services.
The increase in the activities of the centers will lead to increased demand for essential medicines provided or funded by the MOPH and will incur additional administrative burdens on the primary health care department, which will require additional human and financial resources. The expected cost of this initial phase is 60 Billion LBP from which the government will have to contribute with 40 Billion LBP representing only around 6% of the 2013 MOPH budget.
[1] This working paper elaborated in April 2014 was behind the development of the WB project on UHC that started implementation mid 2016.
[2] Director General of the Ministry of Public Health.
Professor at the Faculty of Medicine- Lebanese University
Related video

Sitemap 

- Prevention
- Capacity Building
- Cholera in Lebanon
- Public Health Emergency Operation Center- PHEOC
- Nutrition
- International Health Regulations
- COVID-19 Vaccine
- Novel Coronavirus 2019
- Epidemiological Surveillance
- National Tuberculosis Program
- National AIDS Control Program in Lebanon
- Non-Communicable Diseases
- Communicable Diseases
- No Tobacco Control Program
- Chemical Biological Radio Nuclear Events Preparedness (CBRN Program)
- Health Care System
- Free Medicines Distributed by the Ministry of Public Health
- Infant Formulas (from 0 to 1 year)
- MoPH Tariffs
- Lebanon National Drugs Database
- Primary Health Care
- Expanded Program on Immunization
- Hospital Accreditation
- Public Hospitals
- Admission Criteria Guidelines
- Mother and Child Health
- Pharmaceuticals
- Health Facility Locator
- Elderly Centers
- Local Manufacturing Industries
- Medical Technology
- Narcotics
- Quality & Safety
- Good Manufacturing Practices for Pharmaceuticals in Lebanon
- List of Reference Laboratories
- List of Medications Provided By MoPH in the Catastrophic Disease Management Program
- Pharmacovigilance System in Lebanon
- Government Controls List
- List of Contact Lenses and Solutions for Contact Lenses Approved from MoPH
- Elderly Centers
- List of Authorized IRBs
- Quality Assurance of Pharmaceutical Products
- Drugs National Guidelines
- List of Food Supplements Permitted By MOPH
- List of Bottled Water Permitted by MOPH
- Osteoporosis Assessment and Treatment
- Medical Devices Recalls
- List of Registered Implantable Medical Devices at MOPH
- Blood Transfusion
- Drugs Recalls
- Food Safety
- Education & Awareness
- Health Tips
- Awareness Campaigns
- Communicable Diseases Guidelines: Surveillance and Response
- Countries Requiring Yellow Fever Vaccination for Incoming Travelers
- Ebola Education & Training Materials
- Patients Rights
- Antimicrobial Resistance
- Public Awareness to Prevent Communicable Diseases During the Waste Crisis
- Programs & Projects
- MediTrack Project - Track & Trace System for Pharmaceuticals
- Pandemic Fund Lebanon Project: Using the One Health Approach To Drive Resilience and Recovery
- "Ma3an" Together Against Corona
- Strengthening Lebanon's COVID-19 Response Project in Collaboration with the World Bank
- No Tobacco Control Program
- Lebanon Health Resilience Project in Collaboration with the World Bank
- Policy Support Observatory (PSO)
- Vital Data Observatory
- Chemical Biological Radio Nuclear Events Preparedness (CBRN Program)
- Integration of Malnutrition into Primary Health Care
- EU/IfS Project
- ESPISP II
- Quality Assurance of Pharmaceutical Products
- The National E-Health Program
- Emergency Primary Health Care Restoration Project towards Universal Health Coverage in Collaboration with World Bank
- Integration of Non-Communicable Disease Services within Primary Health Care
- Reproductive Health Services
- Accreditation of Primary Health Care Centers in Lebanon
- The National Mental Health Programme
- Governance
- Health Technology Assessment (HTA)
- Lists of Wealth Declarants
- Distribution of Aid and Medical Assistance to the Hospitals following Beirut Blast on 4/8/2020
- Call for Tenders
- Memberships in International Organisations
- Awards Gained
- MOPH Achievements to Enhance Transparency and Prevent Corruption
- MOPH Committees
- Laws Violation
- Good Governance Program in Lebanon (GGM)
- Conflict of Interests
© Copyrights reserved to Ministry of Public Health 2026





